Cardiac anaphylaxis: A case of acute ST-segment elevation myocardial infarction after IM epinephrine for anaphylactic shock

 Cardiac anaphylaxis: A case of acute ST-“>American Journal of Emergency Medicine 31 (2013) 1157.e1-1157.e3
Cardiac anaphylaxis: A case of acute ST-“>American Journal of Emergency Medicine 31 (2013) 1157.e1-1157.e3
Contents lists available at SciVerse ScienceDirect
American Journal of Emergency Medicine
journal homepage: locate/ ajem
Case Report
Cardiac anaphylaxis: A case of Acute ST-segment elevation myocardial infarction after IM epinephrine for anaphylactic shock
Abstract
A 62-year-old male smoker with no other comorbidities presented to emergency department with systemic anaphylaxis, due to oral diclo- fenac for toothache. He developed acute anterior wall myocardial in- farction following IM epinephrine 1 mg 1:1000. Primary percutaneous coronary intervention was done, which showed a thrombus in the mid left anterior descending artery with no evidence of obstructive coronary artery disease after Thrombus aspiration.
Anaphylaxis to many drugs like nonsteroidal anti-inflammatory drugs and antibiotics can trigger myocardial infarction in patients with or without coronary artery disease called Kounis syndrome. The body distribution of mast cells is quite peculiar; most of them are in the lungs and heart. In the heart, mast cells are distributed perivascularly in close proximity to the myocyte and arterial intima. During ana- phylaxis, the release of prostaglandins, leukotriens, cytokines, and immunoglobulin E stimulates degranulation of these mast cells. In this prothrombotic phase of anaphylaxis, epinephrine potentiates platelet aggregation by increasing adenosine diphosphate and arachidonate- induced thromboxane B2 (T x B2) production.
coronary artery spasm appears to be the main causative mechanism in “cardiac anaphylaxis.” However, on the top of vasoactive reaction, mast cell-derived mediators and epinephrine can cause platelet aggregation leading to thrombotic occlusion of the coronary arteries. So it is advised to start with low dose IM epinephrine 0.3 mg (1:1000) over 5 minutes and repeat after 15 minutes if there is no clinical improvement.
A 62-year-old male smoker with no other comorbidities presented to emergency department at 6 AM with complaints of generalized pruritus and shortness of breath after taking diclofenac for toothache 1 hour back. On examination, pulse was 97/min; blood pressure, 84/
60 mm Hg; jvp, normal; cardiovascular system, unremarkable; respiratory system, rhonchi bilaterally. Electrocardiogram (ECG) had nonspecific changes on arrival (ECG 1).
He complained of chest discomfort following IM epinephrine 1mg (1:1000 dilution) given over 5 min. ECG was suggestive of acute anterior wall ST-elevation MI (ECG 2).
Echocardiography showed hypokinetic apex and mid and apical anterior wall with preserved left ventricular systolic function. He underwent a primary angioplasty, which showed a thrombus in the mid left anterior descending artery. Right coronary artery was normal

ECG 1. Sinus tachycardia at 100/min with nonspecific ST-T changes.
0735-6757/$ – see front matter (C) 2013
1157.e2 K. Tummala et al. / American Journal of Emergency Medicine 31 (2013) 1157.e1–1157.e3

ECG 2. Sinus tachycardia at 110/min with ST segment elevation in V1-V4 and reciprocal ST depression in Leads II,III,AVF.
(Fig. 1). Thrombus aspiration was done. Coronary arteries were free of any flow-limiting disease (Fig. 2).
Post procedure, the patient was stable. His investigations showed: normal fasting plasma glucose, 77 mg/dL; low high-density lipopro- tein cholesterol, 24 mg/dL; total cholesterol, 154 mg/dL; low-density lipoprotein cholesterol, 100 mg/dL; Troponin I, 0.3 ng/mL.
Anaphylaxis is a severe, systemic allergic reaction characterized by multisystem involvement, including skin, airway, vascular system, and gastrointestinal tract. Acute myocardial infarction (MI) following anaphylaxis (“cardiac anaphylaxis”) is rare. Epinephrine causing ST elevation in these anaphylactic patients is even more rare.
Anaphylaxis to many drugs like nonsteroidal anti-inflammatory drugs and antibiotics can trigger myocardial infarction in patients with or without coronary artery disease called Kounis syndrome [1,2]. Degranulation of the mast cells is the primary mechanism in anaphylaxis. The distribution of mast cells in the body is quit peculiar; most of them are in the lungs and heart. In the heart, mast cells are distributed perivascularly in close proximity to the myocyte and arterial intima [3]. During anaphylaxis the release of prostaglandins, leuko- triens, cytokines, and IgE stimulates degranulation of these mast cells.
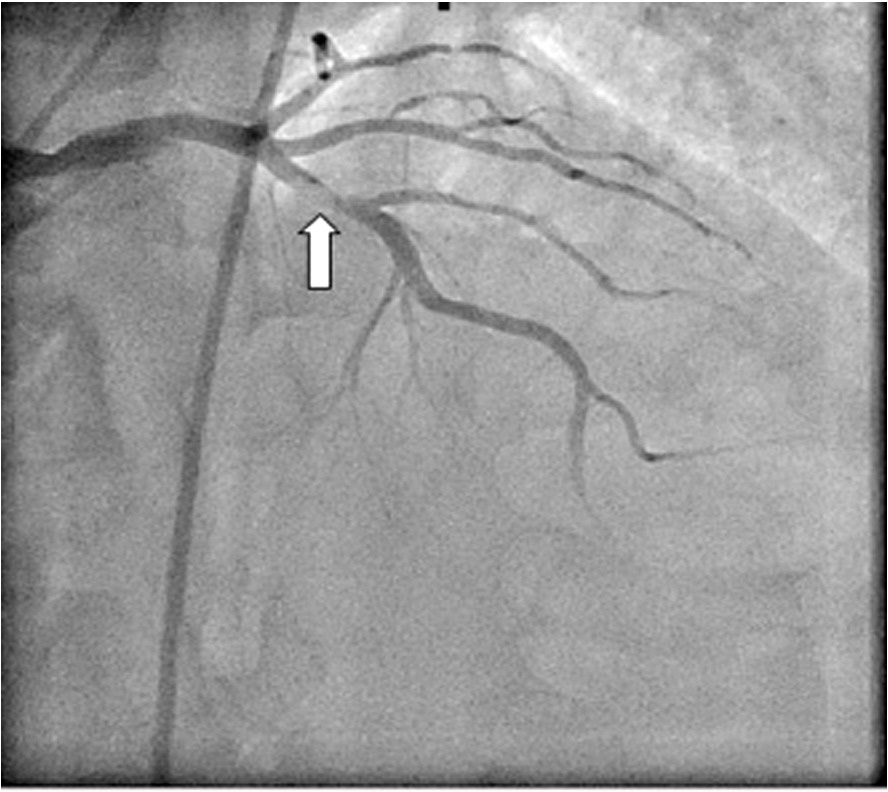
Fig. 1. coronary angiogram was showing a filling defect in the mid left anterior descending artery suggestive of a thrombus.
They release histamine, prostaglandin D2, thrombaxane, and cysteinyl leukotriens [3,4]. Histamine is a potent vasoconstrictor causing vasospasm. Release of these Inflammatory mediators induces coronary artery spasm and/or atheromatous plaque erosion or rupture. In this prothrombotic phase of anaphylaxis, epinephrine potentiates platelet aggregation by increasing adenosine diphosphate and arachidonate- induced thromboxane B2 (T x B2) production [3,4]. The time of presentation of this patient at 6 AM was also important because the Platelet aggregability is the maximum between 6 to 9 AM [5]. In systemic anaphylaxis with hypotension and airway swelling, the recommended dose of IM epinephrine is 0.3 to 0.5 mg (1:1000) given over 5 minutes and repeated every 15 to 20 minutes if there is no clinical improve- ment [6]. In the above case, high-dose epinephrine 1 mg (1:1000) IM has triggered the formation of a thrombus in the left anterior descending artery causing an acute anterior wall myocardial infarction; after thrombus aspiration, there is no residual flow-limiting coronary artery disease.
Coronary artery spasm appears to be the main causative mech- anism in “cardiac anaphylaxis.” On the top of vasoactive reaction, due to mast cell-derived mediators, epinephrine can cause platelet
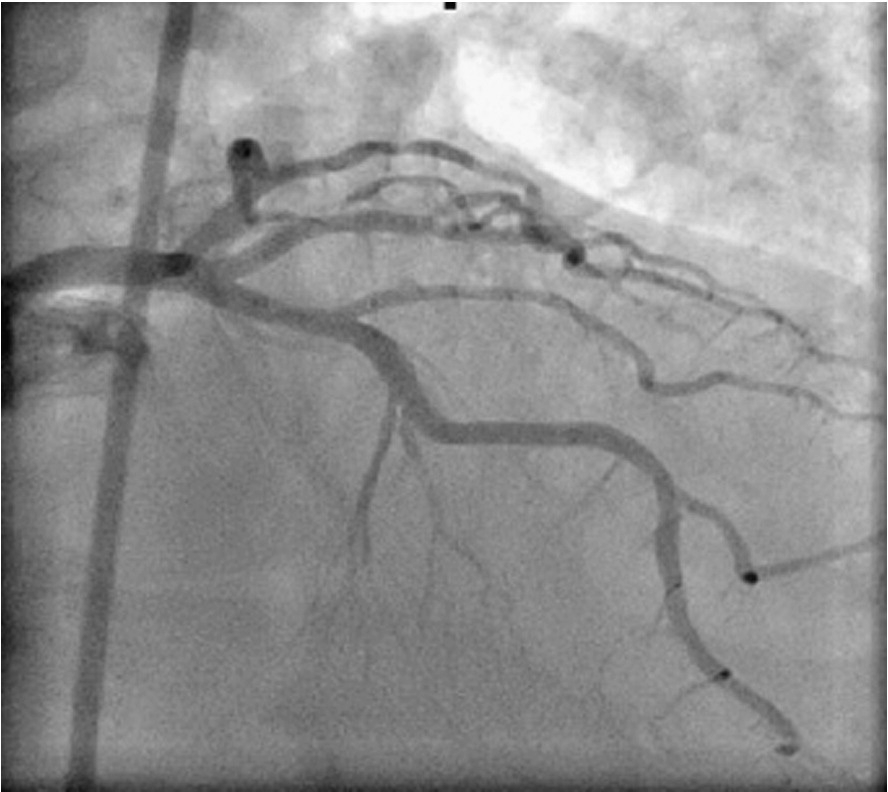
Fig. 2. Coronary angiogram after thrombus aspiration, showing normal left coronary system.
K. Tummala et al. / American Journal of Emergency Medicine 31 (2013) 1157.e1–1157.e3 1157.e3
aggregation leading to thrombotic occlusion of the coronary arteries. So it is advised to start with low-dose IM epinephrine (0.3 mg [1:1000] dilution over 5 minutes) and repeat it after 15 minutes if there is no clinical improvement.
Karthik Tummala MD Vijay K. Maniyal MD, DM
Rajiv Chandrashekaran MD, DM Navin Mathew MD, DM Gaurav Ganeshwala MD
Department of Cardiology, Amrita Institute of Health Sciences
Kochi, India
http://dx.doi.org/10.1016/j.ajem.2013.03.025
References
- De Groot JWB, Gosselink ATM, Ottervanger JP. Acute ST-Segment Elevation Myocardial Infarction Associated With Diclofenac-Induced Anaphylaxis: Case Report. Am J Crit Care 2009;18:388, 386-7.
- Kounis NG. Kounis syndrome (Allergic angina and allergic myocardial infarction): a natural paradigm? Int J Cardiol 2006;110(1):7-14.
- Cameron HA, Ardlie NG. The facilitating effects of adrenaline on platelet aggregation. Prostaglandins Leukot Med 1982;9(1):117-28.
- Sakata V, Komamura K, Hirayama A. Elevation of plasma histamine concentration in the coronary circulation in patients with variant angina. Am J Cardiol 1996;77: 1121-6.
- Tofler GH, Brezinski D, Geoffrey H, Schafer AI, Czeisler CA, Rutherford JD, et al. Concurrent morning increase in platelet aggregability and the risk of myocardial infarction and sudden cardiac death. N Engl J Med 1987;316:1514-8.
- Anaphylaxis. American Heart Association recommendation. Circulation 2005;112 IV-143-IV-145 November 28.
