The accuracy of ultrasound evaluation in foot and ankle trauma
a b s t r a c t
Objectives: Foot and ankle injuries that result in sprains or fractures are commonly encountered at the emergency department. The purpose of the present study is to find out the accuracy of ultrasound (US) scanning in injuries in the aforementioned areas.
Methods: Ottawa Ankle Rules-positive patients older than 16 years who presented to the emergency department with foot or ankle injuries were eligible. For all patients, US evaluation of the whole foot and ankle was performed by an emergency physician before radiographic imaging. All radiographic images were evaluated by an orthopedic specialist and compared with the interpretations of the US.
Results: One hundred thirty-one patients were included in the study. Radiographic evaluation enabled the determination of fractures in 20 patients, and all of these were identified with US imaging. Moreover, US evaluation radiographically detected a silent ankle fracture in 1 patient. The sensitivity of US scanning in detecting fractures was 100% (95% confidence interval [CI], 83.8-100), the specificity was 99.1% (95% CI, 95- 99.8), the positive predictive value was 95.2% (95% CI, 89.6-98), and the negative predictive value was 100% (95% CI, 96.4-100), respectively. The most common fractures were detected at the lateral malleolus and at the basis of the Fifth metatarsal.
Conclusions: Ultrasound imaging permits the evaluation of foot and ankle fractures. Because it is a highly sensitive technique, US can be performed in the emergency department with confidence.
(C) 2013
The most commonly encountered regions of injury in clinical practice are the foot and ankle [1]. The most frequent injury forms in this region occur as buckling or blunt trauma and usually result in a strain, sprain, or, more rarely, fracture [2]. Although such injuries are usually not life-threatening, the affected limb or limb functions can be endangered, and therefore, correct early diagnosis and treatment can prevent long-term complications [3].
Because ultrasound (US) imaging is cheap, is irradiation-free, and permits the evaluation of Soft tissues, it has been of growing importance in foot and ankle injuries [4,5]. In the American College of Emergency Physicians “emergency ultrasound guidelines,” pub- lished in 2001 and 2009, the use of bedside US for emergency physicians has been considered in trauma, Ectopic pregnancy, Abdominal aortic aneurysm, cardiac, biliary and renal diseases, deep vein thrombosis, soft tissues, musculoskeletal body parts, detection of thoracic and ocular pathology, and interventional procedures [6].
Because US is a dynamic analysis method that enables the easy detection of small changes that may occur, it provides the advantage of comparison with the asymptomatic symmetric anatomical body part [7,8]. Acute ankle trauma is an important indication of emergency
* Corresponding author.
E-mail address: [email protected] (S. Ekinci).
US examination, and because it allows for visualizing a large number of joints in a short period, US evaluation gains an advantage over magnetic resonance imaging. In addition, patients acclimate easily to US evaluation. Because it is performed by the same physician who has already examined the patient, it provides quick diagnosis because the physician can rapidly combine images with the patient’s history and clinical status [9,10]. However, there are limited studies and data concerning the standardization of foot and ankle US scan methods and pathological definitions [9]. In these studies, it has been clearly indicated that specific anatomical points (landmarks) on the foot and ankle can be analyzed in detail alongside bone structures through the use of special probe positions, and abnormal situations can easily be diagnosed [7,11,12]. Trinh et al [13] emphasize that detection of lateral ankle fractures with US is highly sensitive.
The purpose of the present study is to determine the accuracy of US scanning in patients with foot and ankle trauma admitted to the emergency department with bone injuries.
- Methods
This study was a prospective evaluation of a diagnostic test (US) vs a reference standard examination (radiography). Informed consent from patients was obtained for all subjects. Our work was approved by the local university institutional review board and was enrolled from May 2011 to June 2012, at the Ankara University School of Medicine, Emergency Department. During the study, the triage nurse made
0735-6757/$ – see front matter (C) 2013 http://dx.doi.org/10.1016/j.ajem.2013.06.008
Criteria for inclusion
- Aged 16 or older
- Conscious and stable patient
- Absence of penetrating trauma
- Absence of Open fractures, dislocations, and major trauma
- Absence of osteomyelitis or chronic problems such as internal fixation
- Positive Ottawa Ankle Rules
- Give written consent before study
Table 2
Bone structures assessed by US
Medial malleolus Navicular
LM Cuneiforms (medial, intermediate, lateral)
Calcaneus Cuboid
Talus MT (1, 2, 3, 4, 5)
contact with the primary physician in charge of the study when a patient with foot or ankle injury presented. In this way, the physician in charge of selecting the patients ensured that they met the inclusion criteria (Table 1) and recorded the patients’ sex, age, the trauma form (sprains or blunt), the cause of the injury (walking, running, sports, or traffic accident), and the buckling mechanism (inversion, eversion).
The physician applying US (primary physician) attended many musculoskeletal US workshops and congresses, as well. Currently, training in US is part of the curriculum of our emergency medicine residency program. Physical examination findings were recorded, and fractures of the bone structures (Table 2) were immediately evaluated by the primary physician in charge.
Ultrasound, applied to all patients, was performed in accordance with the European Society of Musculoskeletal Radiology, Ankle Ultrasound Technical Guidelines [12]. Ultrasonographic examinations were performed before radiography. Ordering necessary radiologic examinations and treatments of the patients were overseen by another physician. The clinician who performed the US did not see the x-rays and x-ray interpretation. Patients with ankle injuries had their ankle anteroposterior and lateral x-rays and Mortis x-ray taken, whereas those with foot injuries had foot anteroposterior and lateral x-rays taken. An oblique x-ray was obtained when injury to metatarsals (MTs) was suspected. In this way, all of the subjects included in the study underwent both ultrasonography and radiog- raphy. At the end of the study, all the radiographic images were interpreted by an orthopedic specialist in terms of fracture, and these were added to the records. The research study protocol did not disrupt the clinical management of patients.
The ultrasonographic images were obtained by a Logiq Book XP (General Electric, Logiq book XP, Turkey) device and a Linear probe (10 MHz). Statistical analysis was performed with SPSS 15 for Windows (SPSS Inc, Chicago, IL).
Table 3
Distribution of injury activities
|
Injury activities |
No. of patients |
% |
|
Walking |
92 |
70 |
|
Running |
21 |
16 |
|
MVA |
6 |
5 |
|
MVPA |
1 |
1 |
|
Sports |
11 |
8 |
|
Soccer |
7 |
5 |
|
Basketball |
2 |
1 |
|
Volleyball |
1 |
1 |
|
Tennis |
1 |
1 |
MVA, motor vehicle accident; MVPA, motor vehicle-pedestrian accident.
Continuous variables are presented as mean and SD, whereas categorical data were presented as frequency and percentage. Comparisons of categorical variables between the groups in terms of ?2 and Fisher exact test for continuous variables between comparison groups were acquired with the Mann-Whitney U test; a P value less than .05 was considered statistically significant. Because radiography is considered the criterion standard, sensitivity and specificity values were calculated for US.
- Results
During the study, a total of 219 patients were admitted with injury in the foot and ankle incurred while walking or running, or during sports activities, or as a result of a traffic accident. Of those, 14 were younger than 16, 5 were unstable, 4 had open fractures or dislocations, 3 had chronic foot or ankle problems, 5 did not want to participate in the study, and 57 were excluded because of failure to comply with Ottawa Ankle Rules . As a result, a total of 131 patients with foot or ankle injuries were included in the study. One hundred three (78.6%) patients had sprains, and 28 (21.4%) presented with blunt trauma.
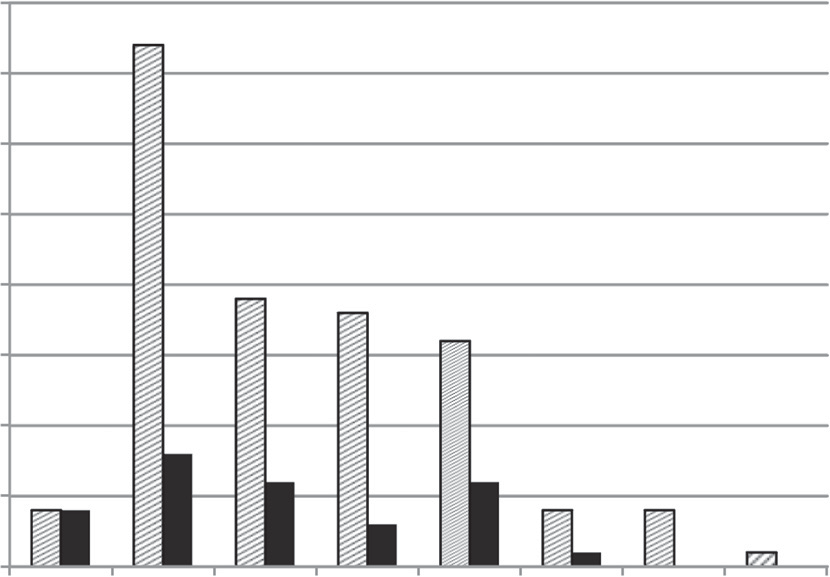
The mean age of all patients was 37.2 +- 15.44 (16-88) years. The mean age of patients with blunt trauma was 34.6 +- 14.66 (17-66) years, and the average age of patients with sprains was 38 +- 15.64 (16-88) years. There was no statistically significant difference between the average age of patients according to trauma forms (P = .261). Graphic 1 shows age ranges and number of patients according to trauma forms. Of all patients, 67 (51.1%) were female and 64 (48.9%) were male. In terms of male/female ratio, there was no statistically significant difference (P = .891) in sprains or blunt trauma forms.
In 92 patients (70.2%), the activity causing the injury (sprain or blunt trauma) was determined to be walking. Twenty-one patients (16%) were injured during running, and 11 patients (8.4%) were injured during sports activities. One patient had a motor vehicle accident (0.8%), and 6 patients (4.6%) were subjected to the trauma of

Fig. 1. A and B, Patient 3. A, US image: bone shown as hyperechoic line. The discontinuity shows the line of fracture zone. B, radiography (foot oblique).
Determination of fractures with radiography findings in bone structures in terms of trauma forms
Figs. 1 through 5. Patient 21 was detected to have a fracture upon x- ray examination 1 week later.
Seven to 10 days after US examination, each patient was reached
Trauma
Bone structures Total
by telephone and asked whether they would prefer to be examined with US in case of a new trauma. One hundred twenty patients (91.6%) could be reached. Of these, 114 patients (95%) stated that they would prefer to be diagnosed with US in case of a new trauma. Two patients (1.7%) answered that they would not, and 4 patients (3.3%) had no preference.
- Discussion
|
forms |
LM |
MM |
Bimalleolar |
5. MT |
4. MT |
2. MT |
||
|
Sprains n |
7 |
2 |
2 |
5 |
1 |
0 |
17 |
|
|
41.2 |
11.7 |
11.7 |
29.5 |
5.9 |
0 |
100 |
||
|
6.8 |
1.9 |
1.9 |
4.8 |
0.9 |
0 |
16.3 |
||
|
Blunt trauma |
n |
1 |
0 |
1 |
0 |
0 |
1 |
3 |
|
%a 33.3 |
0 |
33.3 |
0 |
0 |
33.3 |
100 |
||
|
%b 3.4 |
0 |
3.4 |
0 |
0 |
3.4 |
10.2 |
||
|
Total n 8 |
2 |
3 |
5 |
1 |
1 |
20 |
||
|
%c 40 |
10 |
15 |
25 |
5 |
5 |
100 |
||
|
%d 6.1 |
1.5 |
2.3 |
3.9 |
0.7 |
0.7 |
15.2 |
||
MM, medial malleolus.
a Percentages of patients with fracture in same forms of trauma.
b Percentages of patients in same forms of trauma.
c Percentages of all patients with fracture.
d Percentages of all patients.
the foot or ankle from a motor vehicle-pedestrian accident. Sports causing buckling injuries were determined as soccer (64%), basketball (18%), volleyball (9%), and tennis (9%) (Table 3).
Forty-six (35.1%) of all patients stated that they remembered the mechanism of trauma. Of these, 31 patients had sprains and 15 were exposed to blunt trauma. In patients who remembered the buckling mechanism, 24 (77.4%) had inversion and 7 had eversion injuries.
Fractures were detected in 20 patients (15.2%) by radiography. Seventeen patients (85%) had a fracture as a result of sprains, and 3 (15%) had blunt trauma fracture. The mean age was 39 +- 24.87 (17-66) years in patients with fractures occurring as a result of blunt trauma; the mean age of patients with fracture as a result of buckling was found to be 46.5 +- 16.87 (22-75) years. Patients with fractures were older, and this was statistically significant (P = .009). In patients who had a fracture, 12 (60%) were female and 8 (40%) were male. No statistically significant difference between sex and the occurrence of fracture (P = .389) was found.
Fifty-five percent of fractures were determined at the lateral malleolus (LM). Because some of them also covered bimalleolar fractures, 40% were diagnosed as isolated fractures of the LM. Five MT fractures constituted 25% of all fractures (Table 4). Fracture was detected in 21 patients (16%) by US evaluation. Radiographic evaluation enabled the determination of fractures in 20 patients, all of which were identified with US imaging. Moreover, in 1 patient, US evaluation revealed a fracture, whereas radiographic images were reported as normal. When radiographic examination was taken as the criterion standard, the sensitivity of US scanning in detecting fractures was 100% (95% confidence interval [CI], 83.8-100), the specificity was 99.1% (95% CI, 95-99.8), the positive predictive value was 95.2% (95% CI, 89.6-98), and the negative predictive value was 100% (95% CI, 96.4- 100), respectively (Table 5). Ultrasonography and radiography images of fractures detected in some patients and in patient 21 are shown in
sensitivity and specificity rates for US
Radiographic findings Total Fracture (-) Fracture (+)
Foot and ankle injuries in emergency departments are encoun- tered quite frequently. The ankle is the most commonly injured joint in the human body [14]. Approximately, 5% of emergency department patients present with an acute ankle injury [15]. The most frequent forms of injury at the ankle occur as buckling or blunt trauma and usually result in a strain, sprain, or, more rarely, fracture [2].
Limb functions may be affected in foot and ankle injuries; therefore, early diagnosis, with timely and specifically tailored treatment, will improve the prognosis [3].
Almost all patients admitted to the emergency department with a main complaint of pain in the foot or ankle are exposed to radiographic examinations. Despite the widespread use of OAR, fractures are seen in less than 15% of these patients [16,17]. In studies made, the fracture rate among patients presenting with foot or ankle injury and meeting OAR was reported to be 22% to 39.8% [17,18]. In the present study, a lower fracture rate (15.2%) was established.
Ultrasound is an imaging technique used for many years to examine musculoskeletal tissues [19]. At the end of the 1980s, with its therapeutic energy ranges and its characteristic of causing pain and a tingling sensation in the site of the fracture, US evaluation was introduced to diagnose fractures [20]. ultrasound evaluation has been used for the last 10 to 15 years to assess acute fractures and ligament damage in foot and ankle trauma [21,22]. For a successful US evaluation in terms of experience and the integrity of the whole examination, time will be needed. For Prompt diagnosis, focused US on symptomatic parts of the body is preferable; to avoid leaving any possible diagnosis accountable, routine-wide US examinations are preferred approaches. Jamadar et al [23] showed that many pathological examinations could be diagnosed in distal limbs, such as the foot and ankle, with focused evaluation. In addition to the comprehensive examination, focused US is increasing the rate of diagnoses reported. When symptoms are diffuse or there is another anatomical region with more severe pain, focused US examination may give incorrect results.
In the present study, bone structures in the foot and the ankle were examined with a comprehensive US evaluation. In addition to this, a more detailed examination was performed in areas with intense symptoms.
We reported that ultrasonography sensitivity in detecting frac- tures was 100% (95% CI, 83.8-100) and its specificity was 99.1% (95% CI, 95-99.8). Although there are few studies on the effectiveness of US in detecting foot and ankle fractures, Canagasabey et al [24] demonstrated that US sensitivity and specificity in diagnosing fractures were 90.9% in patients 16 years or older, in this region. As a result of their evaluation of lateral ankle fractures with a group of adult patients in the emergency department, Trinh et al [13] reported in their study that US sensitivity was 100% and specificity was 88.9%. Simanovsky et al [21] emphasized that in pediatric patients, US sensitivity and specificity for detecting ankle fracture were very high (100% and 96%, respectively). Gurgenidze et al [25] stated that US can be used as the criterion standard not only in traumatic injuries of the foot but also in the diagnosis of inflammatory diseases and conditions, such as soft tissue masses, and that the management of further radiologic examination decisions should be given in light of US
|
US Fracture (-) |
n |
110 |
0 |
110 |
|
% |
99.1 |
0 |
84 |
|
|
Fracture (+) |
n |
1 |
20 |
21 |
|
% |
0.9 |
100 |
16 |
|
|
Total |
n |
111 |
20 |
131 |
|
% |
100 |
100 |
100 |

Fig. 2. A and B, Patient 7. A, US image: minimal effusion present in the fractured area. B, Radiography (Mortis).

Fig. 3. A and B, Patient 17. A, US image: nondisplaced fracture line is seen. B, Radiography (anteroposterior).
findings. It has been shown in studies that most ankle fractures were malleolar and 60% to 70% were unimalleolar [26,27]. Among unimalleolar fractures, the most commonly injured part was the Distal fibula [28]. Cakir et al [29] determined 5 MT fractures in 56% of the patients with isolated MT fractures as a result of foot fractures in their study, which included patients older than 16 years. In the present study, the most frequent fractures were seen at LM (55%, isolated LM 40%), followed respectively by 5 MT fractures (25%) and bimalleolar fractures (15%).
In the present study, the US examination was done by 1 physician. As a result, not all patients admitted to the emergency department
with foot or ankle injuries could be included in the study. This is the major limitation of our study. However, owing to the approximately equal day and night working time, we believe that randomization was reached. During our study period, we did not measure the duration of US application. We started the evaluation first by examining the tender part of the limb, followed by an evaluation of all the bone structures. When the probe was placed on a related bone, fracture diagnosis was rapid. However, a specific position of the probe was required; thus, for a comprehensive US examination, this may prolong the examination duration. Because the study involved US followed by radiography for all patients, we were not able to compare the rapidity of diagnosis of one modality vs the other, nor could we quantify the effect of imaging modality on overall length of stay in the emergency department.

Fig. 4. A-C, Patient 20. A and B, US image: degradation of the hyperechoic bone fracture shows a large fracture zone. C, Radiography (anteroposterior).
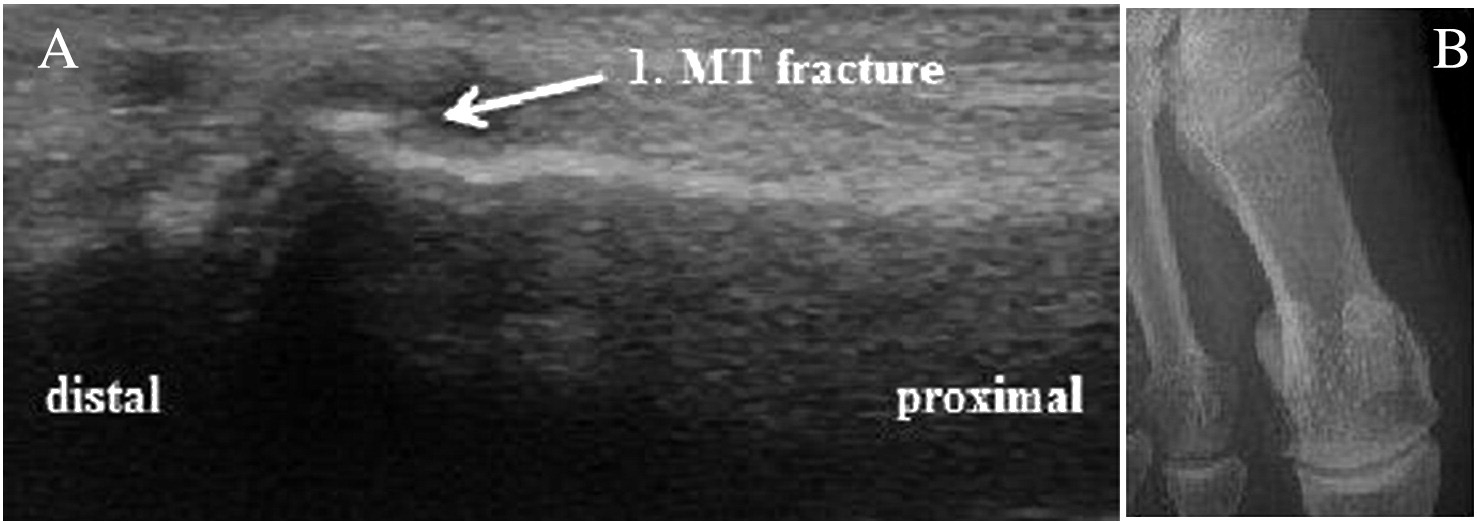
Fig. 5. A and B, Patient 21. A, US image: hyperechoic bone line shows irregularity and minimal effusion. B, Radiography (anteroposterior).
40
35
30
25
No of patients
20
15
10
5
0
16-19 20-29 30-39 40-49
50-59 60-69 70-79 >80
- Rogers CJ, Cianca J. Musculoskeletal ultrasound of the ankle and foot. Phys Med Rehabil Clin N Am 2010;21:549-57.
 Popovic N, Lemaire R. Diagnosis and treatment of acute ruptures of the Achilles tendon current concepts review. Acta Orthop Belg 1999;65:458-71.
Popovic N, Lemaire R. Diagnosis and treatment of acute ruptures of the Achilles tendon current concepts review. Acta Orthop Belg 1999;65:458-71.- American College of Emergency Physicians. ACEP emergency ultrasound guide- lines–2009. Ann Emerg Med 2009;53:500-70.
- Kotnis N, Harish S, Popowich T. Medial ankle and heel: ultrasound evaluation and sonographic appearances of conditions causing symptoms. Semin Ultrasound CT MR 2011;32:125-41.
- Morvan G, Busson J, Wybier M, et al. Ultrasound of the ankle. Eur J Ultrasound 2001;14:73-82.
- Wakefield RJ, Balint PV, Szkudlarek M, et al. Musculoskeletal ultrasound including definitions for ultrasonographic pathology. J Rheumatol 2005;32:2485-7.
- Geusens E, Pans S, Breuseghem IV, et al. Ultrasound in acute trauma of the ankle and hidfoot. Emerg Radiol 2002;9:283-8.
- Maeseneer MD, Marcelis S, Jager T, et al. Sonography of the normal ankle: a target approach using skeletal reference points. AJR Am J Roentgenol 2009;192: 487-95.
- Beggs I, Bianchi S, Bueno A, et al. European Society of Musculoskeletal Radiology,
Age ranges
 Sprain
Sprain  Blunt trauma
Blunt trauma
Graph 1. Age ranges and number of patients according to trauma forms.
In the present study, we investigated the accuracy of US scanning in patients with foot and ankle trauma admitted to the emergency department. In light of our findings during our study, we determined that US scanning is an effective method that can be applied in the emergency department to adult age groups to diagnose foot or ankle fractures. Because US imaging permits the evaluation of bone and because it is irradiation-free, we notice a high rate of satisfaction in patients. In addition, US evaluation can safely be applied in pregnant women and pediatric age groups.
Because the US examination is performed by the same physician who examines the patient, its use in terms of the probability of accurate diagnoses and decisions is of great importance in emergency services triages. Further studies including the evaluation of the effects of US use for the time passed in the emergency department and the diagnosis time in patients with foot and ankle trauma are needed.
- English E. Fractures and soft tissue injuries of the foot and ankle. Can Fam Physician 1985;31:585-90.
- Beynnon BD, Renstrom PA, Alosa DM, et al. Ankle ligament injury risk factors: a prospective study of college athletes. J Orthop Res 2001;19:213-20.
- Geiderman JM, Katz D. General principles of orthopedic injuries. In: Marx JA, Hockberger RS, Walls RM, Adams JG, Barsan WG, editors. Rosen’s emergency medicine: concepts and clinical practice. Philadelphia: Elsevier; 2010. p. 467.
Musculoskeletal Ultrasound Technical Guidelines, VI. Ankle. http://www.essr.org/ html/img/pool/ankle.pdf . (17.06.2012).
- Trinh E, McMillan D, Gough JE, et al. Emergency department use of ultrasonog- raphy to detect lateral ankle fractures. Ann Emerg Med 2004;44:61-2.
- Bauer M, Bengner U, Johnell O, et al. Supination-eversion fractures of the ankle joint: changes in incidence over 30 years. Foot Ankle Int 1987;8:26-8.
- Pijnenburg AM, Glas AS, Roos MAJ, et al. Radiography in acute ankle injuries: the Ottawa Ankle Rules versus local diagnostic decision rules. Ann Emerg Med 2002;39:599-604.
- Brooks SC, Potter BT, Rainey JB. Inversion injuries of the ankle: clinical assessment and radiographic review. BMJ 1981;282:607-8.
- Jenkin M, Sitler MR, Kelly JD. clinical usefulness of the Ottawa Ankle Rules for detecting fractures of the ankle and midfoot. J Athl Train 2010;45:480-2.
- Lucchesi GM, Jackson RE, Peacock WF, et al. Sensitivity of the Ottawa rules. Ann Emerg Med 1995;26:1-5.
- Kane D, Grassi W, Sturrock R, et al. Musculoskeletal ultrasound–a state of the art review in rheumatology. Part 2: clinical indications for musculoskeletal ultrasound in rheumatology. Rheumatology 2004;43:829-38.
- DaCruz DJ, Taylor RH, Savage B, et al. ultrasound assessment of the suspected scaphoid fracture. Arch Emerg Med 1988;5:97-100.
- Simanovsky N, Lamdan R, Hiller N, et al. Sonographic detection of radiographically Occult fractures in pediatric ankle and wrist injuries. J Pediatr Orthop 2009;29: 142-5.
- Fessell DP, van Holsbeeck MT. Foot and ankle sonography. Radiol Clin North Am 1999;37:831-58.
- Jamadar DA, Jacobson JA, Caoili EM, et al. Musculoskeletal sonography technique: focused versus comprehensive evaluation. AJR Am J Roentgenol 2008;190:5-9.
- Canagasabey MD, Callaghan MJ, Carley S. The Sonographic Ottawa Foot and Ankle Rules Study. Emerg Med J 2010;28:838-40.
- Gurgenidze TSh, Mizandari MG, Gadellia GT. Ultrasound in diagnosis of foot lateral aspect pathologies. Georgian Med News 2011;195:26-32.
- Daly PJ, Fitzgerald Jr RH, Melton LJ, et al. Epidemiology of ankle fractures in Rochester, Minnesota. Acta Orthop Scand 1987;58:539-44.
- Court-Brown CM, McBirnie J, Wilson G. Adult ankle fractures–an increasing problem? Acta Orthop Scand 1998;69:43-7.
- Schaffer JJ, Manoli A. The antiglide plate for distal fibular fixation. A biomechanical comparison with fixation with a lateral plate. J Bone Joint Surg Am 1987;69: 596-604.
- Cakir H, Van Vliet-Koppert ST, Van Lieshout EM, et al. Demographics and outcome of metatarsal fractures. Arch Orthop Trauma Surg 2011;131:241-5.