Early vs late fracture fixation in severe head and orthopedic injuries
a b s t r a c t
Background: Patients suffered from craniocerebral trauma with extermities fracture is one of the most common multiple injuries.Actually there is no comparative study demonstrating advantages of early or delayed treatment of skeletal injuries.
Purposes: To conduct a meta-analysis with studies published in full text to demonstrate database to show the as- sociations of perioperative, postoperative outcomes of early fracture fixation(EFF) and late fracture fixation(LFF) for patients with severe head and orthopedic injuries to provide the predictive diagnosis for clinic.
Patients and methods: Literature search was performed in PubMed, Embase, Web of Science and Cochrane Library for information from the earliest date of data collection to October 2017. Studies comparing the perioperative, postoperative outcomes of EFF with those of LFF patients with severe head and orthopedic injuries were includ- ed. Statistical heterogeneity was quantitatively evaluated by x2 test with the significance set P b 0.10 or I2 N 50%. Results: Thirteen papers consisting of 2941 patients were included (1224EFF patients; 1717 LFF patients). The re- sults showed that EFF was related to a greater increase in blood loss, intraoperative blood infusion, crystalloid, hypotension, hypoxia, length of surgery, non-neurologic complications and mortality(P b 0.1). No differences in ICU days, hospital days, neurologic complications and GCS on discharge scores (P N 0.1).
Conclusions: Compared with LFF patients, EFF patients demonstrated an increased risk of perioperative and post- operative complications and clear difference about complications between EFF and LFF about patients with se- vere head and orthopedic injuries.
Level of evidence: Level IV, therapeutic study.
(C) 2018
Introduction
Patients suffered from craniocerebral trauma with extermities frac- ture is one of the most common multiple injuries. A number of studies in orthopedic and neurosurgery literature have supported surgical fixa- tion management of the patient with severe head [1-4]. This early frac- ture fixation has been shown to improve fracture outcome, and reduce perioperative, postoperative complications [5,6].
Recently, the reputed benefits of early fracture fixation have been challenged, study suggested for the first time that early operative stabi- lization may be deleterious in such patients [7-8]. Treatment and pro- tection of the central nervous system is a priority in patients with a significant intracranial trauma. Secondary brain injury may exacerbate underlying head trauma and lead to further morbidity and disability (perioperative and neurologic outcome) [9-11].
Actually there is no comparative study demonstrating advantages of early or delayed treatment of skeletal injuries. Furthermore, the influ- ence of early or delayed treatment in perioperative, postoperative
E-mail address: [email protected] (H. Li).
outcomes of EFF and LFF for patients with severe head and orthopedic injuries is not established. Consequently, it is necessary to perform a comprehensive systematic review and meta-analysis that consists of all the studies to address the question of whether early fracture fixation is safe for patients with severe head injury. Therefore, the purpose of this study was to evaluate the association between EFF,LFF, periopera- tive and postoperative outcomes.
Materials and methods
Literature and search strategy
Two different reviewers independently searched the following elec- tronic databases: PubMed, Embase, Web of Science and the Cochrane Li- brary for information from databases inception to October 2017. The following related terms were searched: early fracture fixation; late frac- ture fixation; patients with severe head and orthopedic injuries; head trauma, intracranial trauma, brain injuries, fractures, fracture fixation, timing; Meta-analysis. Searching strategy was constructed by combin- ing the above terms with “AND” or “OR”. No restrictions were imposed
https://doi.org/10.1016/j.ajem.2017.12.067
0735-6757/(C) 2018

Fig. 1. a. Flow chart illustrating the literature search.
on the language of studies. We had also screened reference lists of re- trieved articles, so that relevant studies were not missed.
Study selection criteria
Two different reviewers independently assessed the retrieved arti- cles to determine whether they met the inclusion criteria. In case of dis- agreements, a third reviewer was involved in the discussion until a consensus was reached. The criteria for inclusion of papers selected for detailed review included the presence of a head injury, the presence of polytrauma, timing of stabilization of the skeleton, neurological as- sessment of patients, and English language. Exclusion criteria included: Case-control studies, animal studies, cadaver studies, single case reports, comments, letters, editorials, protocols, guidelines, publications based on surgical registries, and review papers; for a clinical study, inclusion of fewer than 10 patients.
The patients were divided in the early fracture fixation (EEF) group when fixation took place within 24 h of admission and the late fixation
(LEF) group when fixation was performed later. We analyzed the study type (randomized controlled trial, retrospective review, cohort studies) and treatment methods described. The sample size in each study was extracted from the information available. Injury severity indicators as available were identified and analyzed. These included the Glasgow Coma Scale (GCS), Abbreviated Injury Scores (AIS) for the head and or- thopedic injuries, and the overall Injury Severity Score (ISS). Any com- plications of treatment, the overall length of hospital stay, blood loss intraoperative blood infusion. Infusing intraoperative Crystalloid intra- operative hypotension. Intraoperative hypoxia ICU days, GCS on dis- charge, hospital days and mortality rates were considered.
Data extraction and quality assessment
Two different reviewers independently performed data extraction and methodological quality assessment. Data extracted from the includ- ed studies consisted of authors, publication date, study design, number of patients, and outcome data in both early fracture fixation and late
Summary of the characteristics of the included studies
References Patients ISS GCS Fractures stabilized AIS head AIS orthopedic
|
EFF |
LFF |
EFF |
LFF |
EFF |
LFF |
EFF |
LFF |
EFF |
LFF |
EFF |
LFF |
|||||||
|
Bone 1994 |
676 |
906 |
18-60 |
18-60 |
3-15 |
3-15 |
Any bone |
Any bone |
N/A |
N/A |
N/A |
N/A |
||||||
|
Kalb 1998 |
84 |
39 |
33 |
31 |
9.7 |
9.9 |
Any bone |
Any bone |
4 |
3.9 |
2,9 |
2.6 |
||||||
|
Martens 1988 |
13 |
9 |
37 |
35 |
8 |
8 |
Femur, tibia and pelvis |
Femur, tibia and pelvis |
N/A |
N/A |
N/A |
N/A |
||||||
|
Velmahos 1998 |
22 |
25 |
25 |
23 |
5.8 |
5.7 |
Any bone |
Any bone |
3.8 |
3.4 |
2.9 |
2.4 |
||||||
|
Hofman 1991 |
15 |
43 |
Higher |
Lower |
b 7 |
b7 |
Any bone |
Any bone |
N/A |
N/A |
N/A |
N/A |
||||||
|
Jaicks 1997 |
19 |
14 |
24 |
27 |
11.6 |
10.8 |
Any bone |
Any bone |
3.3 |
3.1 |
3.0 |
2.9 |
||||||
|
Poole 1992 |
46 |
26 |
27.6 |
33.9 |
12 |
10 |
Femur Tibia |
Femur Tibia |
N/A |
N/A |
N/A |
N/A |
||||||
|
Riemer 1993 |
160 |
447 |
23 |
22/26 |
N/A |
N/A |
Pelvis |
Pelvis |
N/A |
N/A |
N/A |
N/A |
||||||
|
Starr 1998 |
14 |
18 |
23.3-32 |
29.8-34.3 |
14.9-6.2 |
13.3-5.6 |
Femur |
Femur |
3.2-4.2 |
3.8-4.1 |
3 |
3 |
||||||
|
Townsend 1998 |
49 |
12 |
Mean |
35 |
b 8 |
b8 |
Femur |
Femur |
N/A |
N/A |
3 |
3 |
||||||
|
Xin Jiang 2014 |
21 |
15 |
24 |
27 |
6.4 |
6.3 |
Any bone |
Any bone |
N/A |
N/A |
N/A |
N/A |
||||||
|
Kotwica 1990 |
51 |
49 |
N/A |
N/A |
Similar |
Similar |
Femur (17) Tibia (27) Pelvis (7) |
Femur (10) Tibia (36) Pelvis (3) |
N/A |
N/A |
N/A |
N/A |
||||||
|
Huangyuan 1999 |
31 |
76 |
N/A |
N/A |
9 |
10 |
Any bone |
Any bone |
N/A |
N/A |
N/A |
N/A |
||||||
|
Yiping 2002 |
23 |
38 |
24 |
27 |
8 |
9 |
Any bone |
Any bone |
N/A |
N/A |
N/A |
N/A |
N/A = not available; EFF = early fracture fixation; LFF = late fracture fixation; ISS = Injury Severity Score; GCS = Glasgow Coma Scale; AIS = Abbreviated Injury Score.
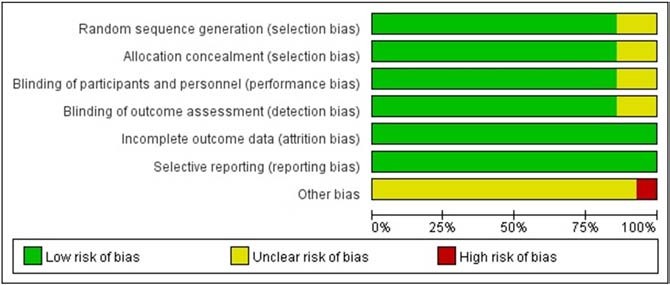
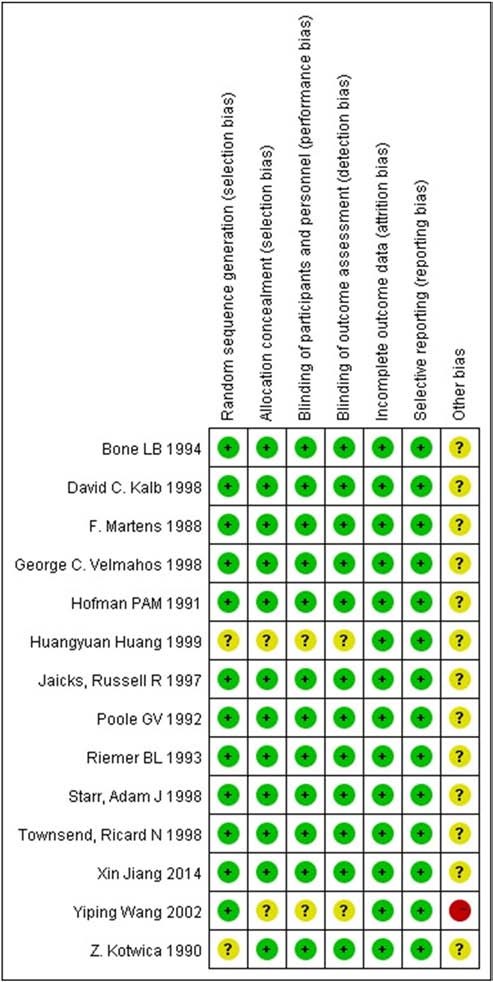
Fig. 3. Risk of bias summary (+ indicates a low risk of bias, – indicates a high risk of bias? indicates unclear or unknown risk of bias).
fracture fixation groups. The outcome measures comprised of the over- all length of hospital stay, blood loss intraoperative blood infusion. In- fusing crystalloid, hypotension, hypoxia, ICU days, hospital days, any complications of treatment and mortality rates were considered. The methodological quality of study was evaluated in seven domains, in- cluding sequence generation, allocation concealment, participants’ blinding, assessors’ blinding, incomplete data, selective reporting and other bias. Each included study could be considered as unclear, low risk or high risk of bias for each domain on the ground of Cochrane Handbook 5.1.0.
Statistical analysis
Statistical analyses were performed using the procedure Review Manager Software 5.3. For dichotomous outcomes, odds ratio (OR) with 95% CI (confidence interval) were calculated to estimate a pooled average difference between EFF with LFF; WMD (weighted mean differ- ences) and 95% CI were calculated for continuous outcomes. Statistical heterogeneity was quantitatively evaluated by Chisquare test with the significance set P b 0.10 or I2 N 50%. The data were presented in the form of Forest plots. Publication bias was assessed by funnel plot.
Results
Literature search
The retrieval strategy is displayed in Fig. 1. Totally, 24 potentially el- igible citations were searched online. After removing duplicate, brows- ing title and abstract and reviewing full text, 14 papers met the inclusion and exclusion criteria [2,12,13,15-17,20,24,26,29,30,32,34,35]. Among all the participants of 14 papers, the outcomes for a total of 2941 pa- tients were described, of which 1224 patients were treated with EFF and 1717 patients with LFF. The detailed characteristics of the studies are listed in Table 1. All 14 were designed as retrospective case reviews of hospital admissions. None used randomization. Two papers were written by neurosurgical units [17,20], two were by orthopedic units [13,26], and three by surgical units [15,16,32]. The remainder included collaboration of all the specialities mentioned above. No other apparent bias was found among the included studies. Figs. 2 and 3 show the risk of bias summary.
Results of the meta-analysis
Three trials reported the details of blood loss. Pooled results showed that EFF was related to a greater increase in blood loss compared with LFF, with WMD = 0.34; 95% CI, 0.27 to 0.41; P b 0.00001, without signif- icant heterogeneity (I2 = 0%, P = 0.40) (Fig. 4).

Fig. 4. Forest plot of comparison: blood loss (EFF; High LFF; CI confidence interval, df degrees of freedom).
Four trials reported the details of intraoperative blood infusion. The results showed that EFF was related to a greater increase in intraopera- tive blood infusion compared with LFF, with WMD = 0.95; 95% CI, 0.74 to 1.15; P b 0.00001, without significant heterogeneity (I2 = 48%, P = 0.10) (Fig. 5).
Four trials reported the details of infusing intraoperative crystalloid. The results showed that EFF was related to a greater increase in infusing intraoperative Crystalloid, with WMD = 1.2; 95% CI, 0.72 to 1.68; P b 0.00001, without significant heterogeneity (I2 = 21%, P = 0.28) (Fig. 6). Four trials reported the details of intraoperative hypotension. The re- sults showed that EFF was related to a greater increase in intraoperative hypotension, with OR = 1.51; 95% CI, 1.06 to 2.15; P b 0.1, without sig-
nificant heterogeneity (I2 = 43%, P = 0.14) (Fig. 7).
Four trials reported the details of intraoperative hypoxia. The results showed that EFF was related to a greater increase in intraoperative hyp- oxia, with OR = 0.53; 95% CI, 0.27 to 1.05; P = 0.03, without significant heterogeneity (I2 = 42%, P = 0.16) (Fig. 8).
Four trials reported the details of length of surgery. The results showed that EFF was related to a greater increase in length of surgery,
with WMD = 1.66; 95% CI, 1.07 to 2.25; P b 0.00001, without significant heterogeneity (I2 = 0%, P = 0.61) (Fig. 9).
Six studies of 354 patients with severe head and orthopedic injuries reported the ICU days and showed no significant difference between EFF and LFF, with WMD = -1.37 95% CI -3.15 to 0.41, P = 0.13, with
moderate heterogeneity (I2 = 79%, P = 0.0003) (Fig. 10).
Five studies reported the hospital days and the results showed that and showed no significant difference between EFF and LFF, with WMD
= -2.23, 95% CI-5.15 to 0.70, P = 0.14, without significant heterogene-
ity (I2 = 0%, P = 0.43) (Fig. 11).
Six studies reported the neurologic complications and showed no significant difference between EFF and LFF, with OR = 0.75, 95% CI
0.42 to 1.35, P = 0.34, without significant heterogeneity (I2 = 30%, P
= 0.21) (Fig. 12).
Seven studies reported the non-neurologic complications and showed EFF was related to a greater increase in non-neuro- logic complications, with OR = 0.64; 95% CI, 0.42 to 0.98; P = 0.04, without significant heterogeneity (I2 = 30%, P = 0.21) (Fig. 13).

Fig. 5. Forest plot of comparison: intraoperative blood infusion (EFF; High LFF; CI confidence interval, df degrees of freedom).
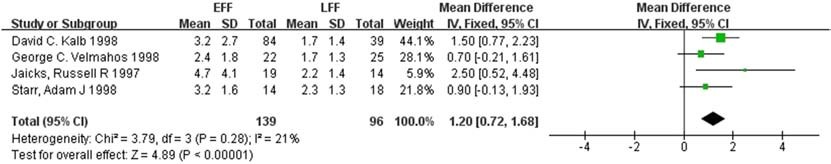
Fig. 6. Forest plot of comparison: infusing intraoperative Crystalloid (EFF; High LFF; CI confidence interval, df degrees of freedom).

Fig. 7. Forest plot of comparison: intraoperative hypotension (EFF; High LFF; CI confidence interval, df degrees of freedom).

Fig. 8. Forest plot of comparison: intraoperative hypoxia (EFF; High LFF; CI confidence interval, df degrees of freedom).

Fig. 9. Forest plot of comparison: length of surgery (EFF; High LFF; CI confidence interval, df degrees of freedom).

Fig. 10. Forest plot of comparison: ICU days (EFF; High LFF; CI confidence interval, df degrees of freedom).

Fig. 11. Forest plot of comparison: hospital days (EFF; High LFF; CI confidence interval, df degrees of freedom).
Eleven studies reported the mortality and showed EFF was related to a greater increase in mortality, with OR = 0.56; 95% CI, 0.44 to 0.73; P b 0.0001, without significant heterogeneity (I2 = 0%, P = 0.81) (Fig. 14). Seven studies reported the GCS on discharge scores and showed no significant difference between EFF and LFF, with WMD = -0.03, 95% CI
-0.50 to 0.44, P = 0.91, without significant heterogeneity (I2 = 0%, P = 0.50) (Fig. 15).
Discussion
Early fracture fixation reduces the noxious stimuli from the fracture site [14]. This is advocated to have a positive effect on the patient’s me- tabolism, muscle tone, body temperature, and thereby cerebral function [18].Furthermore, unstabilized fractures lead to deterioration of the general status of the patient by means of greater soft tissue damage
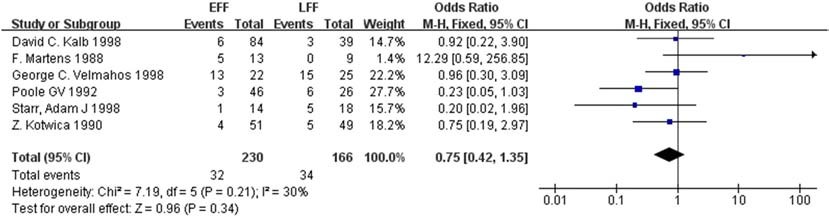
Fig. 12. Forest plot of comparison: neurologic complications (EFF; High LFF; CI confidence interval, df degrees of freedom).

Fig. 13. Forest plot of comparison: non-neurologic complications (EFF; High LFF; CI confidence interval, df degrees of freedom).
and greater risk for Fat embolism, and making nursing care less ef- ficient [19]. These can lead to Respiratory insufficiency and pulmo- nary complications [21] and add to the length of hospital stay [18]. Other authors [22-24] reported that a period of observation after the acute phase of head injury (usually 7 to 10 days) was necessary before operating fracture fixation and could be considered a justifi- able surgical risk, and the risks associated with anesthesia, blood loss and other influence factors are minimized and that this was the safest period for internal fixation of fractures [25-28].
The most important finding of the meta-analysis was that com-
pared with EFF, LFF in patients with severe head and orthopedic in- juries could prevent incidence of mortality and non-neurologic complications and improve clinical outcome in blood loss, intraoper- ative blood infusion, crystalloid, hypotension, hypoxia and length of surgery. LFF was a safe procedure with no significant complications and was highly recommended in patients with severe head and
orthopedic injuries to reduce the incidence of PErioperative and postoperative complications.
A number of studies about the relationship between EFF, LFF, periop- erative, postoperative complications has been published. The commonest time limit for EFF was 24 h [21-24,29]. However, Townsend et al. [30] subdivided their patient group into those operated on in 0 to 2 h, 2 to 12 h, and 12 to 24 h. Bone et al. [2] chose 48 h as the upper limit of the EFF group. It is of note that in two of the studies time limits are not clearly reported [25,26].
During fracture fixation, a risk period for blood loss, intraopera- tive blood infusion, crystalloid, hypotension, hypoxemia, length of surgery, and this will be detrimental to cerebral perfusion and would be an additional insult to the already injured brain, thus outweighing the benefits of EFF and increased incidence of mortality. But both EFF and LFF were well perfused and oxygenated, and there was a similar incidence of intraoperative neurologic complications.

Fig. 14. Forest plot of comparison: mortality (EFF; High LFF; CI confidence interval, df degrees of freedom).
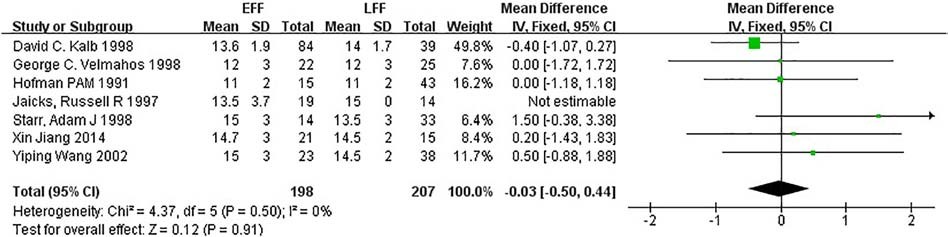
Fig. 15. Forest plot of comparison: GCS on discharge scores (EFF; High LFF; CI confidence interval, df degrees of freedom).
This was achieved by a significant increase in crystalloid and blood infusion in EFF and end organ monitoring of pressure and perfusion [31-33]. These findings suggest that patients undergoing EFF with head injury mandate a management scheme that takes into account blood loss, organ perfusion, pressure and intravascular fluid status to meet specific cerebral organs. Furthermore, patients with com- bined severe head and orthopedic injuries will require length of surgery during early fracture fixation. Also traumatic brain injury is classified as either primary or secondary [34]. Primary injury oc- curs at the time of the accident whereas secondary injury occurs subsequently and is the result of other factors [35]. Head injury is evaluated clinically by the Glasgow Coma Score, which is also pre- dictive of the Variations in the timing of surgery. This study report- ed the GCS on discharge scores and showed no significant difference between EFF and LFF. Therefore the basic tenet of moni- toring cerebral perfusion pressure (CPP) and maintaining intravas- cular fluid status should be continued throughout perioperative, postoperative course [34,35].
Velmahos et al. [32] report a 30% total incidence of pulmonary complications (pneumonia was the commonest followed by ARDS) but found no difference between EFF and LFF. An incidence of 57.7% for the late and 42.2% for the early fixation groups was found by Poole et al. [24] (pneumonia was again the commonest complication but there was no statistical difference). Starr et al.
[29] found a 45 times higher risk of pulmonary complications with delays in fracture fixation (the delayed fixation was a stronger pre- dictor of pulmonary complications than chest injury). During the advancements in surgical instruments and techniques in combina- tion with the progress in perioperative and postoperative critical care has allowed surgeons to repair fractures early. The presumed benefit relied on prevention of Respiratory complications due to early mobilization and more effective pulmonary toilet and nursing care.
The timing of fixation is still under debate for patients with severe Associated injuries and head trauma in particular. Although intraop- erative crystalloid and Blood transfusion requirements were in- creased in the EFF, the intraoperative volume of fluid and overall volume of blood administered during the entire hospital stay was not different. There was no difference in outcome variables between the two groups in ICU days, hospital days, neurologic complications and GCS on discharge were essentially the same between the two groups.
This is a systemic study to report the serious effect of timing of fixa- tion and perioperative and postoperative complications of early fracture fixation and late fracture fixation for patients with severe head and or- thopedic injuries. The most important finding was the clear difference about complications between EFF and LFF. The patients of EFF showed more complications in blood loss, intraoperative blood infusion, crystal- loid, hypotension, hypoxemia, length of surgery and mortality than the LFF patients. Also it appears reasonable that the patient with LFF at least benefits from a thorough analysis of existing comorbidity and optimiza- tion of his or her medical condition, and further higher-quality multi- center prospective studies with good design, large number of participants and long-term follow-up RCTs are necessary to confirm on this topic.
Conflict of interest statement
The authors declare that they have no competing interests.
Ethical review committee statement
The study was approved by the institutional review board of Tianjin Medical University General Hospital, Tianjin, China.
A statement of the location
The work was performed in Tianjin Medical University General Hospital.
References
- Andruszkow H, Schweigkofler U, Lefering R, et al. Impact of helicopter emergency medical service in traumatized patients: which patient benefits most? PLoS One 2016;11:e0146897.
- Bone LB, McNamara K, Shine B, Border J. Mortality in Multiple trauma patients with fractures. J Trauma 1994;37:262-5.
- Buchanan IM, Coates A, Sne N. Does Mode of transport confer a Mortality benefit in trauma patients? Characteristics and outcomes at an Ontario lead trauma hospital. CJEM 2016;18:363-9.
- Bekelis K, Missios S, Mackenzie TA. Prehospital helicopter transport and survival of patients with traumatic brain injury. Ann Surg 2015;261:579-85.
- Cadosch D, Toffoli AM, Gautschi OP, et al. Serum after traumatic brain injury in- creases proliferation and supports expression of osteoblast markers in muscle cells. J Bone Joint Surg Am 2010;92-A:645-53.
- Childs BR, Vallier HA. Cost savings associated with a multidisciplinary protocol that expedites definitive fracture care. Am J Orthop (Belle Mead NJ) 2014;43: 309-15.
- Duncan CM, Moeschler SM, Horlocker TT, et al. A self-paired comparison of peri- operative outcomes before and after implementation of a clinical pathway in patients undergoing total knee arthroplasty. Reg Anesth Pain Med 2013;38: 533-8.
- Dgu T. 20 years TraumaRegister DGU((R)): development, aims and structure. Injury 2016;45(Suppl. 3):S6-s13.
- Desai NK, Kang J, Chokshi FH. Screening CT angiography for pediatric blunt cerebro- Vascular injury with emphasis on the cervical seatbelt sign. Am J Neuroradiol: AJNR 2014;35:1836-40.
- Franz RW, Willette PA, Wood MJ, Wright ML, Hartman JF. A systematic review and meta-analysis of diagnostic screening criteria for blunt cerebrovascular injuries. J Am Coll Surg 2012;214:313-27.
- Gupta AK, Harris JD, Erickson BJ, et al. Surgical management of complex proximal Humerus fractures-a systematic review of 92 studies including 4500 patients. J Orthop Trauma 2015;29(1):54-9.
- Hofman PAM, Goris RJA. Timing of osteosynthesis of major fractures in patients with severe brain injuries. J Trauma 1991;31:261-3.
- Huang Huangyuan, et al. The healing and treatment choosing of fractured patients with coma caused by severe brain injury. The Journal of Bone and Joint Injury 1999;14:297-9.
- Haider AH, Saleem T, Leow JJ, et al. Influence of the National Trauma Data Bank on the study of trauma outcomes: is it time to set research best practices to further en- hance its impact? J Am Coll Surg 2012;214:756-68.
- Jaicks RR, Cohn SM, Moller BA. Early fixation may be deleterious after head injury. J Trauma 1997;42:1-5.
- Kalb DC, Ney AL, Rodriquez JL, et al. Assessment of the relationship between timing of fixation of the fracture and secondary brain injury in patients with multiple trau- ma. Surgery 1998;124:739-44.
- Kotwica Z, Balcewicz L, Jagodzinski Z. Head injuries coexistent with pelvic or lower extremity fractures-early or delayed osteosynthesis. Acta Neurochir 1990;102: 19-21.
- Kadhim HJ, Duchateau J, Sebire G. Cytokines and brain injury: invited review. J Inten- sive Care Med 2008;23:236-49.
- Lozano R, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012;380:2095-128.
- Martens F, Ectors P. Priorities in the management of polytraumatised patients with head injury: partially resolved problems. Acta Neurochir 1988;94:70-3.
- Morley J, Marsh S, Drakoulakis E, Pape HC, Giannoudis PV. Does traumatic brain in- jury result in accelerated fracture healing? Injury 2005;36:363-8.
- Narotam PK, Morrison JF, Nathoo N. Brain tissue oxygen monitoring in traumatic brain injury and major trauma; outcome analysis of a brain oxygen-directed thera- py. J Neurosurg 2009;111:672-82.
- Nahm N, Como JJ, Wilber JH, et al. Early appropriate care: definitive stabilization of femoral fractures within 24 hours is safe in most multiply injured patients. J Trauma 2011;71:175-85.
- Poole GV, Miller JM, Agnew SG, Grisworld JA. Lower extremity fracture fixation in head injured patients. J Trauma 1992;32:654-9.
- Russell K, Meeuwisse W, Nettel-Aguirre A. Comparing the characteristics of snow- boarders injured in a terrain park who present to the ski patrol, the emergency de- partment or both. Int J Inj Control Saf Promot 2014;21:244-51.
- Riemer BL, Butterfield SL, Diamond DL, et al. Acute mortality associated with injuries to the pelvic ring: the role of early patient mobilisation and external fixation. J Trau- ma 1993;35:671-7.
- Raj R, Siironen J, Kivisaari R. Factors correlating with delayed trauma center admis- sion following traumatic brain injury. Scand J Trauma Resusc Emerg Med 2013;21: 67.
- Shan L, Skaggs DL, Lee C, et al. Intensive care unit versus hospital floor: a compara- tive study of postoperative management of patients with adolescent idiopathic sco- liosis. J Bone Joint Surg Am 2013;95(e40):1-5.
- Starr AJ, Hunt JL, Chason DP, et al. Treatment of femur fracture with associated head injury. J Orthop Trauma 1998;12:38-45.
- Townsend RN, Lheureau T, Protetch J, et al. Timing fracture repair in patients with severe brain injury (Glasgow coma scale score b9). J Trauma 1998;44: 977-83.
- Tracy ET, et al. Pediatric injury patterns by year of age. J Pediatr Surg 2013;48: 1384-8.
- Velmahos GC, Arroyo H, Ramicone E, et al. Timing of fracture fixation in blunt trau- ma patients with Severe head injuries. Am J Surg 1998;176:324-7.
- Vercruysse GA, Friese RS, Khalil M, et al. Overuse of helicopter transport in the min- imally injured: a health care system problem that should be corrected. J Trauma Acute Care Surg 2015;78:510-5.
- Jiang Xin, et al. Investigation on operation timing of limb fractures combined with severe craniocerebral trauma in children. China J O ~ hop Trauma 2014;27:486-90.
- Wang Yiping, et al. The best time of operation for fractured patient with craniocere- bral trauma coma. Medical theory and Practice 2002;15:401-2.
