Prehospital amputation: An experimental comparison of techniques
a b s t r a c t
Objective: Prehospital limb amputation is a rare but potentially life-saving intervention. When patients cannot be extricated due to limb entrapment or have Hemodynamic compromise that precludes a prolonged extrication, they may benefit from an emergent prehospital amputation. The objective was to experimentally compare three prehospital amputation techniques on porcine legs.
Methods: The three techniques studied were a scalpel with a Gigli saw, a hacksaw, and a reciprocating saw. For the first technique, a scalpel was used to make a circumferential incision in the soft tissue and a Gigli wire saw to cut through the bone. The second and third techniques only used a saw and did not require soft tissue incision with a scalpel. Three providers including an emergency medicine physician, a paramedic, and a medical student performed three amputations of each technique, resulting in twenty-seven total amputations. The primary out- come was amputation time. Secondary outcomes were rate of instrument malfunction and cleanliness of cut. Results: The primary outcome of amputation time was different between techniques. The Gigli saw technique took 32.86 +- 16.53 s (mean +- SD), hacksaw technique 6.28 +- 0.76 s, and reciprocating saw technique
2.84 +- 0.40 s. There were no differences in amputation time between participants for a given amputation tech- nique. The Gigli saw technique had an instrument malfunction on 3/9 trials which was distinct from the other techniques. Differences in cleanliness of cut were nonsignificant. Conclusions: Prehospital limb amputation with a hacksaw or reciprocating saw may result in faster completion of the time-sensitive procedure with fewer instrument malfunctions.
(C) 2019
Introduction
Background
Prehospital limb amputation is a rare but potentially life-saving in- tervention. When patients cannot be extricated due to limb entrapment or have hemodynamic compromise that precludes a prolonged extrica- tion, they may benefit from an emergent prehospital amputation. Anal- ysis of 132 publicly accessible emergency medical services (EMS) protocols revealed only 15% provide treatment recommendations for prehospital amputation, 6% provide an amputation protocol, and 2% listed specific equipment needed [1]. Further investigation revealed many departments utilize a scalpel and a Gigli saw as their instruments of choice for prehospital amputation [2-7].
Scalpels and Gigli saws are routinely employed in hospital Operating rooms; however, a Gigli saw is an instrument that emergency medicine physicians may not have encountered in their residency training.
* Corresponding author.
E-mail address: [email protected] (J.D. Stilley).
Furthermore, the use of a Gigli saw is not included in standard para- medic curriculum. This lack of training may result in prehospital pro- viders having limited familiarity with this piece of equipment. Conversely, the hacksaw and reciprocating saw are likely to be more fa- miliar to Prehospital providers as they are standard equipment on fire and rescue apparatus. These instruments are not traditionally used to perform an extremity amputation; however, they have utility in a life vs. limb scenario. The limited, if any, surgical training of prehospital pro- viders will inherently result in a non-sterile procedure regardless of the instruments used, supporting exploration into the efficacy of alternative amputation instruments [8].
Previous literature
Literature on the topic is sparse and overwhelmingly limited to case reports and articles describing patients who have had a prehospital am- putation [9-16]. Furthermore, only one experimental trial comparing amputation instruments has been conducted [17]. Leech and Porter ex- plored prehospital-friendly methods of amputation on human cadavers with four different instruments. While having high external validity due
https://doi.org/10.1016/j.ajem.2019.09.002
0735-6757/(C) 2019
to the use of human cadaveric limbs, only one attempt per instrument was performed which may limit the reproducibility in real-world applications.
Goals of this investigation
The objective of this study was to experimentally compare three prehospital amputation techniques on porcine legs by comparing stan- dard equipment to equipment that is more likely familiar to the prehospital team. The primary outcome was amputation time. Second- ary outcomes were rate of instrument malfunction and cleanliness of cut.
Methods
Study design and setting
This study was conducted in the Russell D. and Mary B. Shelden Clin- ical Simulation Center located at the University of Missouri School of Medicine in Columbia, MO, USA. Three participants performed amputa- tions in the study: a board-certified emergency medicine physician who serves as the assistant EMS medical director, a state-licensed paramedic with 30 years of public safety experience, and a second-year medical student with three years of EMT-Basic experience. None of the users had previously performed a prehospital amputation.
Porcine legs were a gift from the University of Missouri Comparative Medicine Program and the Russell D. and Mary B. Shelden Clinical Sim- ulation Center. Porcine legs were chosen due to their availability as un- used components from other studies and their frequent use in orthopedic literature as a human limb analog. Twenty-seven specimens were harvested from animals that had an average weight of 65 kg. The specimens were a combination of front and hind legs amputated at the middle extremity joint, analogous to a human knee joint. Unlike humans, porcine animals are quadrupeds, therefore the anatomic com- position of both sets of extremities are comparable. The specimens were separated into plastic bags and placed in a freezer for preservation. The legs were thawed completely for 24 h prior to the initiation of the study to ensure realistic tissue density. No gross disturbances in soft tissue or bone were identified after thawing, and tissue breakdown after a short period of freezing would not be expected. An adjustable wooden sup- port stand was designed to provide a stable and consistent surface to perform the amputations (Fig. 1). The stand secured both ends of each porcine leg so that the participants could perform a mid-leg amputation through the distal extremity bone, analogous in location to a human tibia, but with the thickness of a femur.

Fig. 1. An adjustable wooden support stand was created to secure porcine legs during amputation trials. The support stand can be adjusted for leg length as well as distal and proximal leg circumference independently.
Techniques
Three amputation techniques were evaluated in the study (Fig. 2). Gigli Saw Technique (GST) involved a scalpel and Gigli wire saw similar to the techniques described in published prehospital amputation litera- ture [2-7]. In this technique, a disposable #10 blade safety scalpel was used to make a circumferential incision in the soft tissue and a Gigli wire saw was used to cut through bone. Participants were required to engage the scalpel blade cover prior to transitioning to the Gigli saw to maximize participant safety. Hacksaw Technique (HST) and Recipro- cating Saw Technique (RST) did not require soft tissue incision with a scalpel. In HST, each participant was instructed to place the hacksaw blade on the skin and use long cut strokes. In RST, each participant was instructed to identify the location of their cut, hold the trigger on the reciprocating saw until the blade reached maximum speed, then perform the amputation.
Efforts were made to use equipment readily available and familiar to fire and rescue services. The hacksaw and reciprocating saw are stan- dard equipment on fire and rescue apparatus. A reciprocating saw is an electrically driven device. Fire and rescue apparatus are able to sup- ply power via inverter or generator for the saw to function. Alterna- tively, the reciprocating saw itself may be battery powered. To decrease confounding variability, the hacksaw blades (M.K. Morse, Can- ton, OH, #HHCB1214-2) and reciprocating saw blades (M.K. Morse, Canton, OH, # RBFR96214WT03) used in this study were the same brand, composed of the same metal alloy, and had the same number of teeth per inch. The reciprocating saw blade is designated as a Fire &

Fig. 2. Three types of amputation equipment were used in this experiment. A. Gigli Saw Technique (GST): Smith & Nephew 12? spiral Gigli saw blade (reference number 210482) with standard ruler to highlight length of wire, Ambulance Service Gigli saw handles (product number PV.270.4.40), disposable Bard-Parker Safety Scalpel #10 (manufacturer number 372610). B. Hacksaw Technique (HST): Tool Shop brand hacksaw (model number 2443911), 12? Morse blade with 14 teeth per inch (product number HHB1214T10). C. Reciprocating Saw Technique (RST): Rockwell 12A corded reciprocating saw (product number RK3637K), 9? Morse Fire & Rescue blade with 14 teeth per inch (product number RBFR96214W).
Rescue blade, which is designed specifically for heavy-duty multipur- pose cutting.
The three techniques were separated into three trials of three ampu- tations each (N = 27 total amputations). GST trials were performed first, HST trials second, and RST trials last. Participant order within the trials was randomized. After every trial (three amputations), new equipment was introduced to prevent excessive instrument wear (i.e. after GST Trial 1, the scalpel and Gigli saw were replaced). A total of three scalpels, three Gigli saw blades, three hacksaw blades, and three reciprocating saw blades were used.
Measurements
A downward-facing camera was strategically placed above the ad- justable wooden support stand, and a continuous video feed of the ex- perimental trials was recorded. Review of the footage allowed for precise timing of each amputation. Manual timing with a stopwatch was performed as a backup if technical difficulties arose with the video recording software. Time was measured from first contact of the blade with soft tissue until completion of cut.
Following amputation trials, images were taken of the proximal as- pect of each leg to aid in measurement of the shortest and longest diam- eters of the cross section (Fig. 3). Cross-sectional area of the cut, bone diameter, and tissue depth to bone was determined using ImageJ Soft- ware (National Institutes of Health, Bethesda, Maryland). Two indepen- dent investigators utilized the freehand and straight-line tools with the scale adjusted to in-image standard rulers.
Post-amputation grading of cleanliness of cut was performed on the proximal aspect of the amputated legs. Cleanliness of cut grading was based on four metrics: soft tissue, tendon, bone, and skin. For soft tissue, tendon, and bone, a specimen could be classified as having 0, 25%, 50%, 75%, or 100% area of disturbance. Skin defects were graded on an integer system by counting the number of gross irregularities. Defects were de- fined as ragged or torn skin due to imprecise shearing of soft tissue. Three members of the research team were responsible for performing the post-amputation grading. One oversight member selected one spec- imen at a time and asked two grading members to evaluate the distur- bance. A consensus between the two grading members was established for each of the measurements. The oversight member subsequently re- corded the measurements and selected another specimen until all spec- imens were evaluated.
Analysis
Data was analyzed for normality and statistical differences using Prism software (GraphPad Software, Inc., La Jolla, CA). A two-way Anal- ysis of Variance (ANOVA) was used to evaluate the Time x Partici- pant x Equipment relationship. No statistical differences were
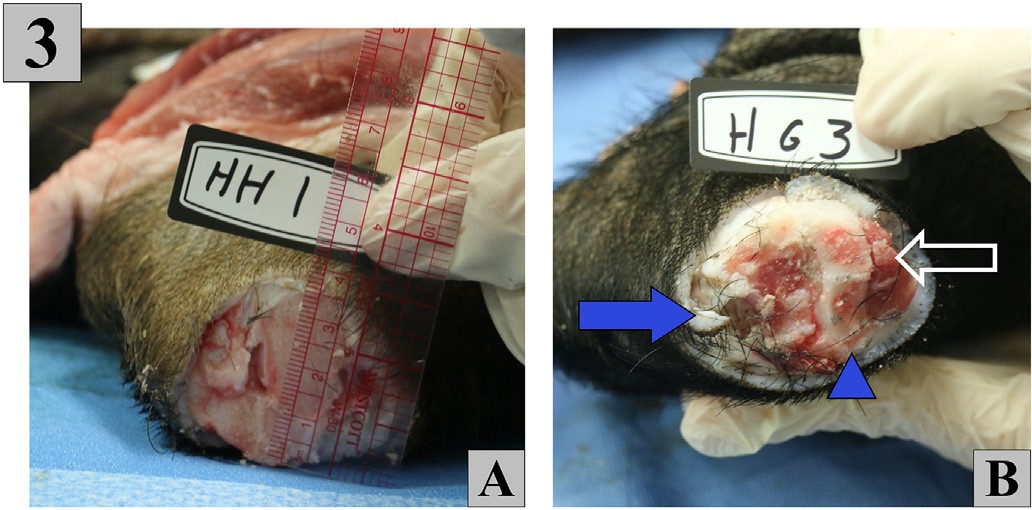
Fig. 3. Cross sectional images of the proximal aspect of each limb were taken. A. Shortest and longest diameters were measured to determine average cross-sectional area. B. A representative image shows defects after cut with scalpel and Gigli saw. Full blue arrow shows skin defect from scalpel, blue arrowhead shows bone chipping, and open white arrow shows soft tissue damage.
detected between participants; therefore, participants were pooled for further analysis. Kruskal-Wallis ANOVA with multiple comparisons were used to detect differences among equipment. Statistically signifi- cant differences were defined as those with a P value of b 0.05 and dif- ferent letters indicate significant differences between groups.
Results
Main results
Our primary outcome of amputation time was different between techniques (p b 0.001, Fig. 4A). GST took 32.86 +- 16.53 s (mean +- SD), HST 6.28 +- 0.76 s, and RST 2.84 +- 0.40 s.
Our secondary outcome evaluating instrument malfunction showed a difference between techniques (p = 0.047, Fig. 4B). GST had an instru- ment malfunction on 3/9 trials. HST and RST did not have any instru- ment malfunctions. The first malfunction in the GST trials occurred with the scalpel. While making a circumferential incision in the soft tis- sue, the scalpel blade fragmented and broke, compromising the safety of the participants. This malfunction was likely due to excessive pressure from contact with the underlying bone while the participant was mak- ing the soft tissue incision. The second and third malfunctions occurred with the Gigli saw itself. The second malfunction occurred as a result of a misaligned circumferential incision which did not completely incise all of the soft tissue. After the Gigli saw had cut through the entire bone, it became stuck on the remaining soft tissue and the scalpel was needed to complete the amputation. The final malfunction occurred as the par- ticipant was approximately halfway through sawing the bone. The wire saw broke into two pieces at the middle of the blade, and the participant was subsequently unable to complete the amputation until a new Gigli saw was obtained.
Secondary outcomes involving cleanliness of cut metrics were largely inconclusive (Table 1). No significant differences were found be- tween groups when comparing measures of bone disturbance (p = 0.096), soft tissue disturbance (p = 0.341), tendon disturbance (p = 0.077), or skin defects (p = 0.114). However, when looking at multiple comparisons for each measure, some minor differences were found. Bone disturbance of HST was slightly improved compared to RST (p = 0.034), and tendon disturbance of GST was slightly improved com- pared to HST (p = 0.041). No other differences were detected among any of the groups.

Fig. 4. Graphs displaying statistically significant primary and secondary outcomes. A. Differences in time to complete the amputation were detected. RST performed the amputation the quickest compared to HST or GST. The GST required more time to complete the amputation and with greater variability (data are represented as minimum to maximum boxes with a line representing the mean. Differing letters above the bar indicate significance). B. Secondary measures of instrument malfunction rates detected differences. GST had a greater rate of instrument problems than the other amputation techniques (data are represented as minimum to maximum boxes with a line representing the mean. Differing letters above the bar indicate significance).
Cleanliness of cut by each amputation technique. Data represented as mean +- SD.
|
GST |
HST |
RST |
|
|
% Bone Disturbed |
36.1 +- 28.3 |
19.4 +- 24.3 |
44.4 +- 24.3 |
|
% Soft Tissue Disturbed |
55.6 +- 34.9 |
33.3 +- 35.4 |
44.4 +- 27.3 |
|
% Tendon Disturbed |
25.0 +- 28 |
56.3 +- 29.1 |
52.8 +- 31.7 |
|
# Skin Defects |
1.3 +- 1.0 |
0.7 +- 0.5 |
1.2 +- 0.4 |
Post-amputation analysis with ImageJ software was performed, and the results of the two investigators were averaged (? = mean 97.1% be- tween measurements). The average cross-sectional area of the porcine legs was calculated to be 22.0 +- 5.1 cm2. Bone diameter averaged
5.0 +- 2.4 cm2 with soft tissue comprising a mean 77% of the cross- sectional surface area. Average tissue depth to reach bone was 3.1 +-
1.4 mm.
Discussion
Limitations
This study does have its limitations. In the foremost, porcine limbs are not human limbs. Porcine skin has been shown to be a good model for human skin [18]. However, the relative lack of muscle and ad- ipose tissue in the porcine specimens may not have been representative of human patients. This difference may have allowed the hacksaw and reciprocating saw to more easily shear the soft tissue without clogging the saw teeth. Therefore, the findings in this study may have variable application to humans depending upon the soft tissue composition of the patient. Yet, similar to the findings of Leech and Porter on human skin, the use of other amputation methods improved time to procedure completion, lending further support for using porcine skin as a human analogue [17].
Repeated use of equipment may have caused instrument failures. Amputation instruments were replaced at the end of every trial (every three amputations) to prevent excessive wear. However, one could argue the scalpel or Gigli saw failures in GST were due to an unrealistic repetitive use of the instruments. While a valid consideration, the scal- pel and Gigli saw malfunctions occurred before their third amputation of the trial. Furthermore, due to routine environmental challenges in the prehospital environment, it is important to choose equipment capa- ble of holding up to hard use in non-ideal circumstances.
The adjustable wooden support stand created for this experiment provided a secure and level surface to perform the amputations. This was done in order to minimize confounding variability between the am- putation equipment. Unfortunately, prehospital providers are infre- quently able to control the positioning of a patient’s limb during emergent amputation and must adapt to situations of entrapment with access difficulty.
Clinical significance
Prehospital limb amputation using the Hacksaw Technique (HST) or Reciprocating Saw Technique (RST) are superior to the Gigli Saw Tech- nique (GST) for amputation time and may result in fewer instrument malfunctions. We hypothesize the time difference will have greater clinical significance when extrapolated to human legs. According to the National Health Statistics Report of 2008, the average calf circumfer- ence in males 20 years of age and older is 39.5 cm [19]. When this cir- cumference is used to estimate cross-sectional area, it reveals a value of 124.2 cm2. This is a greater than 500% increase in cross sectional area as compared to the porcine legs used in this experiment. Extrapo- lating from our data, we speculate it would take on average 185 s to per- form a mid-calf amputation on an average human with GST, 35 s with HST, and 16 s with RST. The difference between the fastest and slowest techniques is 169 s, just shy of three minutes. In a time-critical
resuscitation with a hemodynamically unstable patient, this extra time may lead to adverse outcomes.
This study was performed on porcine legs in a controlled environ- ment with proper Personal protective equipment, limiting exposure to communicable disease. The biohazard risk associated with performing a rapid prehospital amputation on humans cannot be overstated. Pro- vider safety should be held in the utmost regard, and every effort should be taken to limit spread of bodily tissues and fluids. The study by Leech and Porter concluded that amputation with a reciprocating saw pro- moted significant blood splatter [17]. Additionally, an unprotected scal- pel or saw blade would increase injury risk. When choosing which amputation instruments to use, provider safety is an important consid- eration. Personnel involved in a field amputation must take ample pre- cautions to prevent Accidental exposure or injury.
All instruments used in the amputation techniques functioned via a shear stress mechanism. Shear stress limits anatomic damage away from the site of amputation by directing force parallel to the blade. However, the inherent lack of sterility and precision of cut in a prehospital amputation would necessitate operative revision. Any de- tectable differences in cleanliness of cut between GST, HST, and RST are unlikely to impact the effectiveness of the operative revision or the overall outcome of the procedure. Further investigation may warrant deeper analysis of cleanliness of cut metrics and the extent of operative revision required between techniques.
Beyond the quantifiable measures of time and malfunction rate, the HST and RST provide superiority to the GST in field-limb-access. In the field, only one provider may be able to gain access to the patient at a time, often with inconvenient positioning [12,20]. The GST requires wide 360? limb access to perform the circumferential soft tissue incision and to wrap the Gigli saw around the bone. Additionally, this technique requires two hands in close proximity to the site to manipulate the saw. In real-world circumstances, this level of access to the entrapped limb may not be feasible [20]. In contrast, the HST and particularly the RST only require a forward cutting surface to complete the amputation. The HST does require open space behind the limb to allow for full cut- ting motion. Other cutting instruments with a smaller physical footprint may also be of value, such as a small battery-operated bone saw or ro- tary saw. However, a bone saw would still require 360? limb access for skin and soft tissue excision with a scalpel, and a rotary saw may take more time to complete the amputation. Further investigation that sim- ulates entrapment with access difficulty may be warranted.
Meetings
Poster presentation at American Academy of Emergency Medicine Scientific Assembly in Las Vegas, NV on 3/22/2019.
Poster presentation at Health Sciences Research Day at the Univer- sity of Missouri School of Medicine in Columbia, MO on 11/15/2018.
Author contributions
JDS was responsible for the design and oversight of the study. BWE, CSS, and BGH were the three participants in the study. JAWS oversaw data collection and performed data analysis. KEP and JAWS performed grading of limb disturbance. BWE drafted the manuscript, and all au- thors contributed to its revision. JDS is the corresponding author and takes responsibility for the paper as a whole.
Funding/grants
This research did not receive any specific grant from funding agen- cies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
None.
The authors would like to acknowledge the Russell D. and Mary B. Shelden Clinical Simulation Center at the University of Missouri School of Medicine for the kind use of their experimental laboratory space, video recording equipment, and project conception suggestions.
References
- EMS protocols. Acid remap, LLC. www.emsprotocols.org/. Accessed June 20, 2019.
- Zils S, Codner P, Pirrallo R. Field physician manual. Medical College of Wisconsin; 2011.
- Mustafa IA. Field limb amputations. In: Seminole County (Florida) Fire Department.
- Medical operations manual. In: Rescue M-DF, editor. Protocol 31 – field crush ampu- tation kit; 2016.
- Porter KM. Prehospital amputation. Emerg Med J 2010;27(12):940-2.
- Cortez E, Keseg DP, Augustine JJ. EMS field amputation protocols for urban & non- urban envirnoments. JEMS 2016.
- Roberts KJ. The role for surgery in pre-hospital care. Trauma 2015;18(2):92-100.
- Kampen K, Krohmer J, Jones J, Dougherty J, Bonness R. In-field extremity amputa- tion: prevalance and protocols in emergency medical services. Prehosp Disaster Med 1996;11(1):63-6.
- Bunyasaranand JC, Espino E, Rummings KA, Christiansen GM. Management of an entrapped patient with a field amputation. J Emerg Med 2018;54(1):90-5.
- Pust G, Grossman M, Shatz D, et al. The rare requirement of on-scene extremity am-
putation in the entrapped trauma patient. Panam J Trauma Crit Care Emerg Surg 2016;5(2):93-100.
Macintyre A, Kramer EB, Petinaux B, Glass T, Tate CM. Extreme measures: field am- putation on the living and dismemberment of the deceased to extricate individuals entrapped in collapsed structures. Disaster Med Public Health Preparedness 2012;6: 428-35.
- Sharp CF, Mangram AJ, Lorenzo M, Dunn EL. A major metropolitan “field amputa- tion” team: a call to arms and legs. J Trauma 2009;67(6):1158-61.
- Kohn M, Mechem CC. EMS field amputation gives trauma patient a second chance at
Walker B. Crash victim’s leg amputated in ‘unprecedented’ North Idaho rescue. Idaho Statesman 2017.
- Yang C, Ross W, Peterson M. Prehospital field amputation leads to improved patient outcome. JEMS 2018.
- Escott MEA. Field amputation protocols useful when man gets trapped in tree. JEMS 2016.
- Leech C, Porter K. Man or machine? An experimental study of prehospital emer- gency amputation. Emerg Med J 2016;33(9):641-4.
- Bronaugh RL, Steward RF, Congdon ER. Methods for in vitro percutaneous absorp- tion studies II. Animal models for human skin. Toxicol Appl Pharmacol 1982;62 (2):481-8.
- McDowell MA, Fryar CD, Ogden CL, Flegal KM. Anthropometric reference data for children and adults: United States, 2003-2006. National Health Statistics Reports 2008;10:1-45.
- Ho JD, Conterato M, Mahoney BD, Miner JR, Benson JL. Successful patient outcome after field extremity amputation and cardiac arrest. Prehospital Emergency Care 2003;7(1):149-53.
