Point-of-care ultrasound may expedite diagnosis and revascularization of occult occlusive myocardial infarction
a b s t r a c t
Background: Electrocardiographically occult occlusive myocardial infarction (OOMI), defined as coronary artery occlusion requiring revascularization without ST-segment elevation on electrocardiogram (ECG), is associated with delayed diagnosis resulting in higher morbidity. Left ventricular (LV) wall motion abnormalities (WMA) ap- preciated on echocardiography can expedite OOMI diagnosis. We sought to determine whether point-of-care ul- trasound (PoCUS) demonstrating WMA expedites revascularization time when performed on emergency department patients being evaluated for OOMI.
Methods: This was a single-site retrospective cohort study over a 38-month period. All admitted adult ED patients
>=35 years of age evaluated by the emergency physician with PoCUS for LV function, an ECG, and a standard tro- ponin I biomarker assay were included. Patients with ST-segment elevation myocardial infarction , prior LV dysfunction, fever >=100.4 ?F, or hypotension were excluded. A structured chart abstraction was performed for relevant demographic and clinical characteristics.
Results: We screened 1561 ED patients who underwent cardiac PoCUS for eligibility: 874 met exclusion criteria, 453 were discharged, and 234 were included in the analysis. Twenty-three patients had coronary interventions, of which 14 had WMA. PoCUS was performed 36 min (IQR -9-68) before troponin resulted (n = 234) and 39 min (IQR -23-96) before the first Troponin elevation (n = 85). Twenty of the 23 patients diagnosed with OOMI had elevated troponins prior to catheterization with time from PoCUS to first troponin elevation of 43 min (IQR 9-263). Of these patients, 11 had WMA identified on PoCUS, and the WMA was appreciated 47 min (IQR 26-255) prior to troponin elevation. The time from ED arrival to revascularization was 673 min (IQR 251-2158); 432 min (IQR 209-1300) among patients with WMA (n = 14) compared with 2158 min (IQR 552-3390) for those without WMA (n = 9).
Conclusion: Cardiac PoCUS may identify OOMI earlier than standard evaluation and may expedite definitive man- agement.
(C) 2022
Occlusive myocardial infarction is defined as acute coronary artery occlusion requiring revascularization. This can occur with or without ST-segment elevation on electrocardiogram (ECG) [1]. In the latter, this electrocardiographically occult occlusive myocardial infarction (OOMI) can be associated with significant delays to catheterization and reperfusion, as well as high morbidity [1]. In the setting of any oc- clusive myocardial infarction, reperfusion is paramount to salvage
* Corresponding author at: Department of Emergency Medicine, 263 Farmington Ave, Farmington, CT 06032, United States of America.
E-mail address: [email protected] (M.K. Herbst).
myocardium at risk of infarction, and delays to treatment can negatively affect outcomes [2]. Among the earliest manifestations of cardiac ische- mia are hypokinesia and dyskinesia of the left ventricle (LV) found on echocardiography [3]. regional wall motion abnormalities (WMA) ap- preciated on Point-of-care ultrasound performed by emer- gency physicians in the Emergency Department (ED) may identify these electrocardiographically occult Ischemic events earlier than the current standard of care [4,5].
The aim of this study was to determine whether PoCUS expedites re- vascularization time for patients with WMA. To do this, we measured the time between PoCUS performance and first elevated troponin result among ED patients being evaluated for OOMI. We then compared the time to catheterization and coronary revascularization based on the
https://doi.org/10.1016/j.ajem.2022.06.010
0735-6757/(C) 2022
presence of WMA on PoCUS among ED patients presenting with symp- toms concerning for acute coronary syndrome (ACS) but without ST- segment elevation myocardial infarction (STEMI) on ECG.
- Methods
- Study design
This was a single-site retrospective cohort study at an academic medical center of all patients presenting to the ED who received a car- diac PoCUS exam during their ED visit. The study data were collected over a 38-month period, from May 1, 2018 to June 30, 2021. Institu- tional Review Board approval was obtained from the study institution, and consent was waived for this study.
-
- Study setting and population
The study site was a Level III academic suburban ED designated as a STEMI-receiving center with an annual census of approximately 38,000 patients and 20 emergency medicine attending physicians. The ED has a three-year Emergency Medicine residency training program with 54 residents and a four-year medical university on campus, as well as an active PoCUS training program for residents and students. There are two Fuji Sonosite Xporte (Bothell, WA) ultrasound machines available for clinical use at all times. Faculty can bill for PoCUS and are encour- aged, but not required, to incorporate PoCUS into clinical care to guide diagnosis and management decisions. All PoCUS images undergo qual- ity assurance performed by a single ultrasound fellowship-trained emergency physician.
-
- Patient selection
All adult ED patients >=35 years of age who had an ECG, a standard troponin I biomarker assay, and a cardiac PoCUS examination per- formed by the clinical emergency physician to assess LV function during the study period were included. Patients with an ECG demon- strating STEMI, known prior LV dysfunction, or any documented fever
>=100.4 ?F or hypotension (mean arterial pressure < 65 mmHg) during the ED visit were excluded. Presence of a STEMI was noted on the ECG documentation portion of the ED visit or in the medical decision- making portion of the visit note. Prior LV dysfunction was defined as a previously documented systolic cardiomyopathy, WMA or an ejection fraction <55% reported by the patient or documented prior to the date of the ED visit in the electronic medical record (EMR). Additionally, pa- tients with prior myocardial infarction were included if a subsequent echocardiogram documented an ejection fraction of 55% or above and no WMA, but otherwise were excluded.
-
- Data collection
The study period crossed both a non-automated and automated PoCUS workflow [6]. Using DICOM data for the non-automated period and an EMR report for the automated period, a list of all patients who re- ceived cardiac PoCUS examinations in the ED during the study period was used as the basis for the chart review. Exclusion criteria were ap- plied, and a structured chart abstraction was performed for relevant demographic and clinical characteristics. The chart abstraction was conducted by four investigators using a case review form. Discrepancies were adjudicated independently by two separate investigators. A subset of 10% of charts were reviewed by a fifth investigator to ensure accuracy. Study variables included ED arrival time, PoCUS acquisition time, presence of WMA on PoCUS, order and result time of initial troponin biomarker assays, and result time of the first elevated troponin bio- marker assay. If a left heart catheterization was performed within one week of the patient’s ED presentation, the date, time, result, and inter- vention documented in the interventional cardiology note were also in- cluded as study variables. For patients who underwent coronary artery bypass graft (CABG), we assigned the time of revascularization as the time of cardiac catheterization. Timestamps for ED arrival time, tropo- nin biomarker assay order and result times, and catheterization result were obtained from the EMR. PoCUS acquisition time was defined by the timestamp on the first PoCUS image acquired. The cardiac PoCUS in- terpretations were entered in real time by the emergency physicians who acquired the images and were responsible for the clinical care of
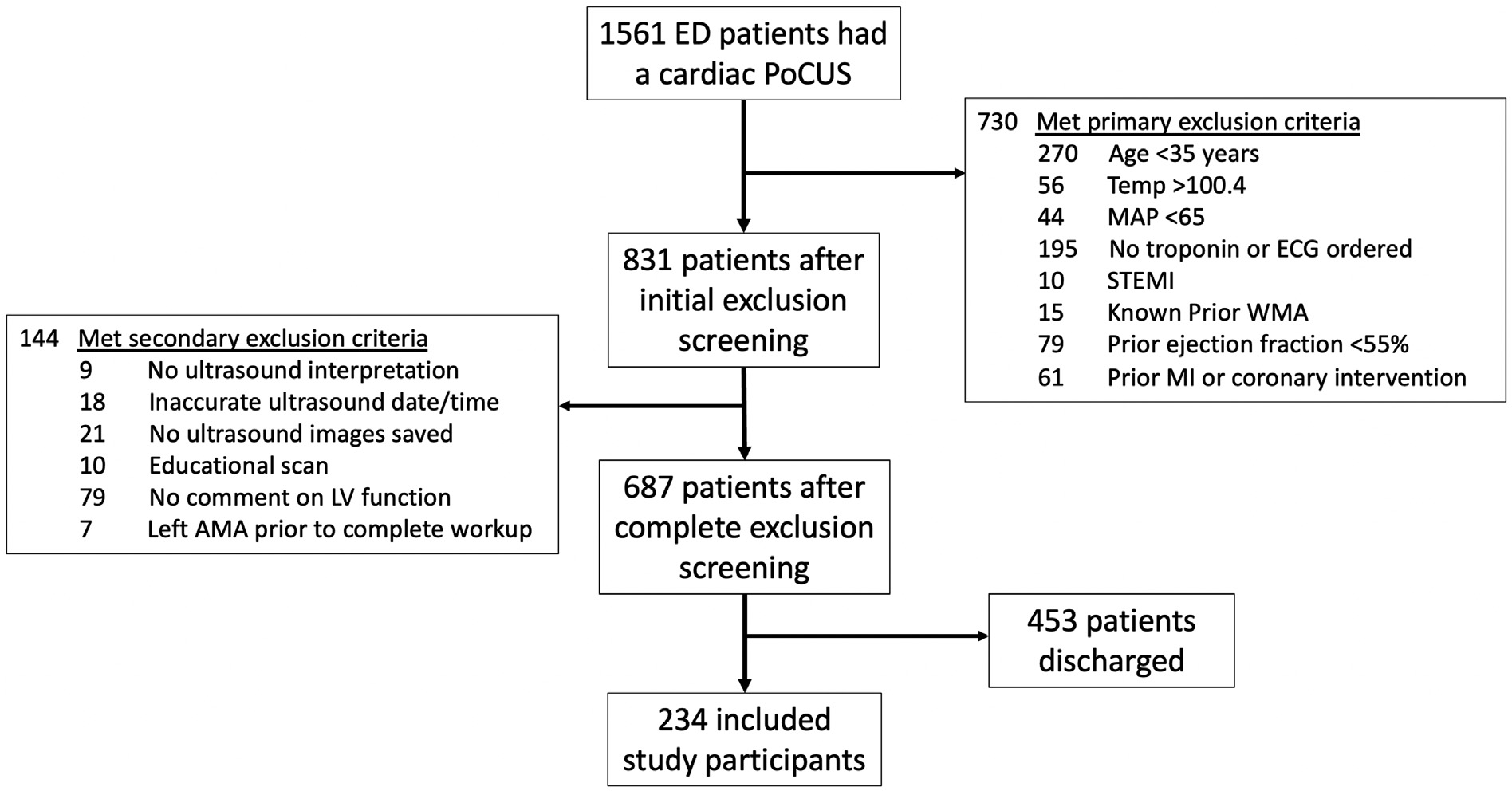
PoCUS, point-of-care ultrasound; LV, left ventricle; AMA, against medical advice; Temp, temperature in degrees Fahrenheit; MAP, mean arterial pressure; STEMI, ST-elevation myocardial infarction; WMA, Wall motion abnormality; MI, myocardial infarction.
Patient demographic and clinical characteristics.?
discharged from the ED, and 234 met inclusion criteria and were in- cluded in the analysis (Fig. 1). Patients included had a median age of
Study population (N = 234)
Not revascularized (N = 211)
Revascularized (N = 23)
Significance
69.5 years. Eighty-five patients had an elevated troponin during their hospitalization. Nineteen patients had a WMA on PoCUS. Thirty-nine patients (16.7%) had a left heart catheterization within one week of
Age – yr 69.5 +- 15.7
69.7 +- 16.1 67.9 +- 12.3 NS
the ED visit, of which 23 were diagnosed with OOMI requiring revascu- larization. Average HEART (history, ECG, age risk factors, and troponin)
Female Sex – % 50.0 51.7 34.8 NS
score was 4.5 +/- 1.7. Table 1 compares the average HEART score of
Race/Ethnicity –
P = patients with OOMI requiring revascularization to patients who did not require revascularization.
A cardiac PoCUS examination was performed before the first tropo-
|
no. (%) |
0.0461?? |
|||
|
Asian |
7 (3) |
6 (2.8) |
1 (4.3) |
|
|
Black |
33 (14.1) |
32 (15.2) |
1 (4.3) |
|
|
Hispanic |
23 (9.8) |
23 (10.9) |
0 |
|
|
White |
170 (72.6) |
149 (70.6) |
21 (91.3) |
nin biomarker result time for 168 patients, and after the first troponin biomarker result time for 65 patients. Median time between the order
HEART Score??? 4.5 +- 1.7 4.2 +- 1.6 6.4 +- 1.3 P < 0.0001
* Plus-minus values are means +-SD.
?? Race and ethnicity were obtained from the medical record registration information. P– value is for the comparison between white vs. non-white patients (Fisher’s exact test).
??? HEART score for Major adverse cardiac events is generally stratified into low risk
(0-3), intermediate risk (4-6), and high risk (7-10).
the patient. During the nonautomated period, presence of WMA was documented on the ultrasound machine and saved as a still image. Lack of documentation of a WMA was interpreted as “no WMA”. During the automated period, data regarding PoCUS WMA was already dichot- omized as present or absent, with the option to indicate the hypokinetic region in the EMR. Troponin biomarker elevation was defined as greater than or equal to 0.05 ng/mL.
-
- Measuring outcomes and data analysis
We used Microsoft Excel (Microsoft Corp.) and MedCalc Statistical Software version 19.7.4 (MedCalc Software Ltd., Ostend, Belgium; https://www.medcalc.org; 2021) for time interval measurements and de- scriptive statistics for all variables. Proportions were compared using a chi square analysis. Medians were compared using a Wilcoxon Rank Sum test. A Log-rank (Mantel-Cox) test was used to compare the time to cath- eterization of patients with and without WMA to revascularization.
Overall, 1561 patients underwent a cardiac PoCUS in the ED over the 38-month study period. Of these, 874 met exclusion criteria, 453 were
and result time of the initial troponin biomarker was 62.5 min (IQR 49-85). Median time from PoCUS performance to first troponin result was 35.5 min (IQR -9.0-68.0).
Fig. 2 illustrates the time in minutes from ED arrival to key results. PoCUS was performed 36 min (IQR -9-68) before troponin resulted (n = 234) and 39 min (IQR -23-96) before the first troponin elevation (n = 85). Twenty of the 23 patients diagnosed with OOMI had elevated troponins prior to catheterization with time from PoCUS to first tropo- nin elevation of 43 min (IQR 9-263). Of these patients, 11 had WMA identified on PoCUS, and the WMA was appreciated 47 min (IQR 26-255) prior to troponin elevation.
Fourteen (61%) of the 23 patients with final diagnosis of OOMI had WMA. Characteristics between those with WMA and those with- out WMA can be seen in Table 2. Among these patients, the median time from ED arrival to revascularization was 673 min (IQR 251-2158)], 432 min (IQR 209-1300) among patients with WMA compared with 2158 min (IQR 552-3390) for those without WMA, p = 0.006 (Fig. 3).
Of the 19 patients that had WMA on PoCUS in our study popula- tion, 18 had a left heart catheterization. Fourteen had a final diagnosis of OOMI requiring revascularization, two had Takotsubo cardiomyopathy, one had 65% left circumflex occlusion without in- tervention, and one had clean coronaries. The latter two had a final diagnosis of congestive heart failure. The only patient with WMA who did not go to the catheterization laboratory had a final diagnosis of chronic obstructive pulmonary disease exacerbation. Table 3 sum- marizes patients with WMA and their respective catheterization findings where applicable, as well as patients without WMA diag- nosed with OOMI.
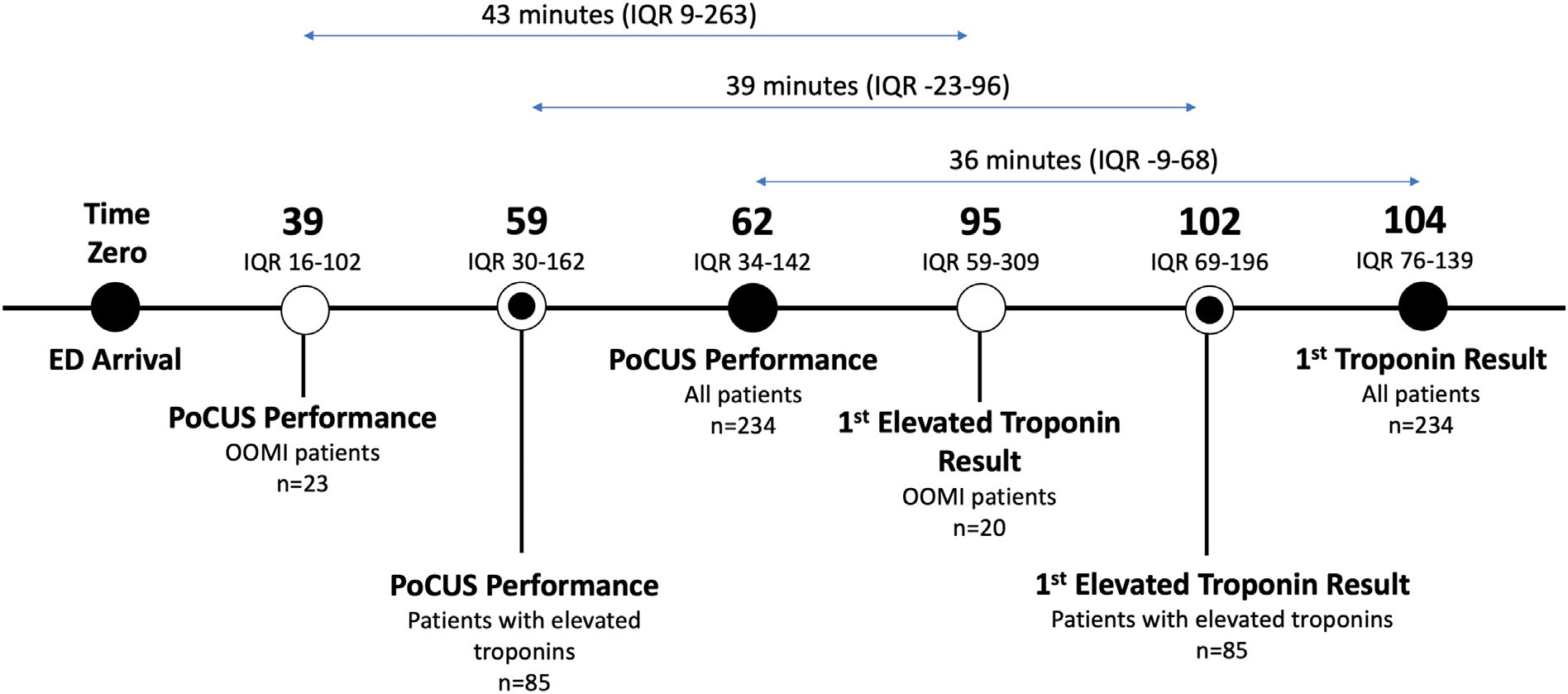
Fig. 2. Median time in minutes from Emergency Department arrival to point-of-care ultrasound performance and first troponin results in different patient subsets. ED, Emergency Depart- ment; PoCUS, point-of-care ultrasound; OOMI, occult occlusive myocardial infarction; IQR, interquartile range.
Characteristics of revascularized patients according to the presence or absence of WMA.?
Table 3
Description of wall motion abnormalities found by emergency physicians and their re- spective catheterization findings where applicable.
WMA present
WMA absent
Significance
|
(N = 14) |
(N = 9) |
Case |
WMA PoCUS |
Catheterization findings |
|||
|
Age – yr |
67.5 +- 12.5 |
68.6 +- 11.3 |
NS |
1 |
None |
95% LAD |
|
|
Male – no. (%) |
8 (57) |
7 (78) |
NS |
2 |
None? |
Multivessel; 80% LMA, 80% Ramus Intermedius |
|
|
HEART Score?? |
6.4 +- 1.3 |
6.5 +- 1.4 |
NS |
3 |
Anterior |
99% LAD |
|
|
Arrival to PoCUS – mins |
36 (11-55) |
40 (17-161) |
NS |
4 |
None? |
Multivessel; 90% LAD, 80% RCA |
|
|
median (IQR) |
5 |
None? |
Multivessel; occluded RCA, severe obtuse marginal, |
||||
|
First Troponin Elevated – no. (%) |
9 (64) |
6 (67) |
NS |
severe mid-LAD |
|||
|
CABG – no. (%) |
1 (7) |
2 (22) |
NS |
6 |
Anterior |
90% LAD |
* Plus-minus values are means +-SD.
|
7 |
None? |
100% LAD |
|
8 |
Anterior |
Proximal LAD thrombus |
|
9 |
Lateral |
85% LCX |
|
10 |
Anterior |
Severe mid-LAD |
|
11 |
None |
Multivessel; 80-90% LAD, 20-30% distal LAD, 60% LCX, |
|
12 |
Anterior |
70-80% proximal RCA Severe 70% distal left main coronary artery extending |
|
into the ostial LAD |
?? HEART score for major adverse cardiac events is generally stratified into low risk (0-3), intermediate risk (4-6), and high risk (7-10).
- Discussion
To our knowledge, this is the first study to look at how emergency physician-performed PoCUS in patients with nondiagnostic ECGs suspected of having OOMI may impact the time to revascularization. Our results support that a WMA appreciated on PoCUS performed by emergency physicians may be the earliest indication of OOMI requiring revascularization, up to hours before an elevated troponin result. Fur- thermore, the presence of a WMA on PoCUS was associated with a sig- nificantly shorter time from ED admission to catheterization compared to revascularized patients without a WMA.
Our results build upon other studies supporting that detection of WMA not only occurs among STEMI patients, but also among NSTEMI patients, potentially identifying higher-risk patients that would benefit from revascularization (type I NSTEMI) and differentiating them from patients who would not benefit from revascularization (type II NSTEMI) [4,7]. In this way, WMA can contribute to the differentiation between type I and type II NSTEMI patients, both of which require elevation of troponin [8]. In the absence of STEMI on ECG, waiting for troponin ele- vation delays prompt revascularization [9]. In our study, many patients, including several with OOMI requiring revascularization, had a negative initial troponin result.
Many departments have adopted high sensitivity troponin as- says to improve early detection of OOMI, rather than the conven- tional assay which was used in this study. While this may lead to earlier ACS rule-out in some patients, it is at the cost of more ele- vated results that may obscure which patients need immediate catheterization [10]. Even using the conventional assay, only 27% of patients with elevated troponin in our study had OOMI that
- Anterior 98% LAD
- Anterior 99% LAD, 90% LCX
- Apical 90% proximal LAD
- Anteroseptal 95% LAD
- Anterior 100% LAD
- None 70% LAD, 60% RCA
- Apical 90% RCA
- Inferior Occluded mid-RCA
- Anterior 99% LAD
- None 90% ostial LCX lesion
- None Multivessel
- Septal No catheterization, COPD exacerbation
- Septal 65% LCX
- Septal Near-normal coronaries, 45% EF, diffuse hypokinesis
- Anterior Takotsubo cardiomyopathy
- Inferior/posterior Takotsubo cardiomyopathy
LAD, left anterior descending artery; CABG, coronary artery bypass graft; LCX, left circum- flex; RCA, right coronary artery; LMA, left marginal artery; CHF, congestive heart failure; EF, ejection fraction.
* Reduced left ventricular function.
required revascularization. Similarly, Aslanger et al. found that only 28.2% of NSTEMI patients had an acute coronary occlusion, supporting the poor specificity of the NSTEMI nomenclature [11]. While elevated troponin is sensitive, these assays took time and did not always predict the need for revascularization in our study population. We attempted to exclude patients with fever or hypo- tension who might have had elevated troponin due to demand, such as sepsis, hemorrhage, or other shock states, to better capture
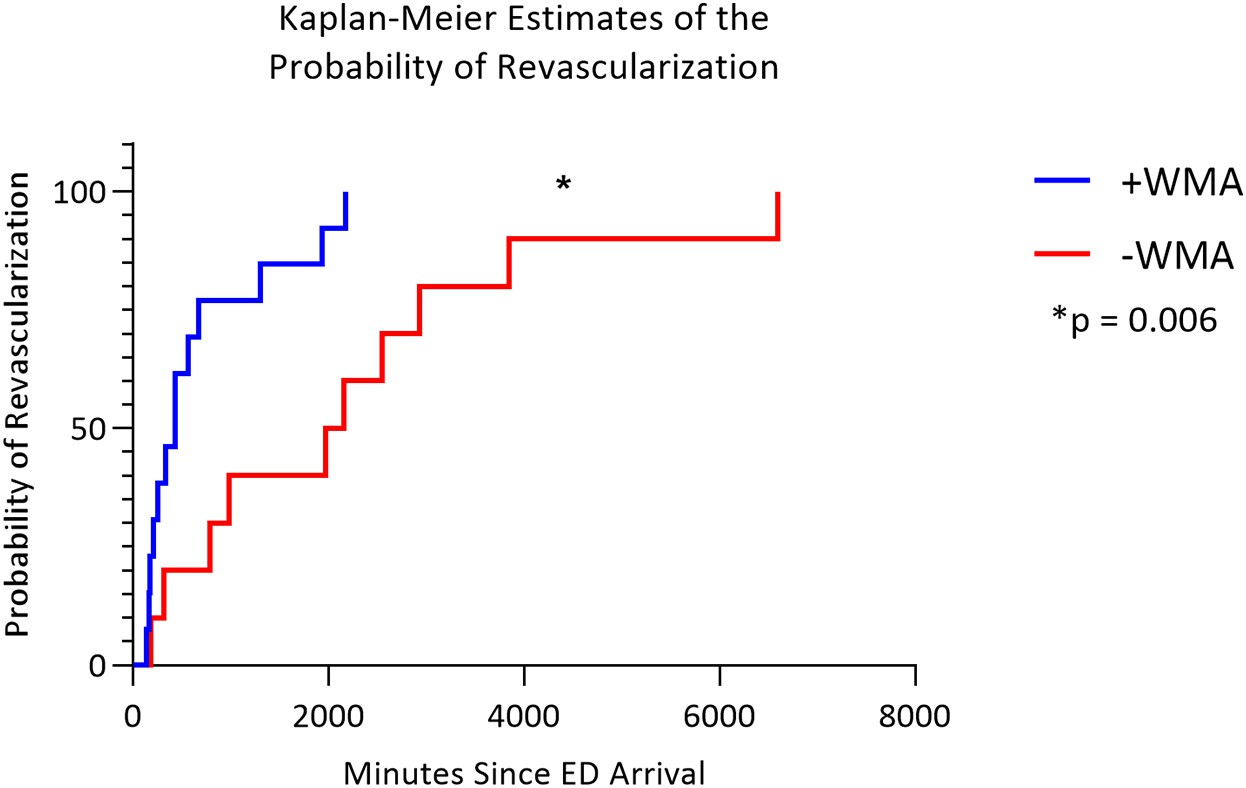
Fig. 3. Kaplan-Meier estimates of the probability of revascularization according to presence or absence of a wall motion abnormality on point-of-care ultrasound among patients who un- derwent catheterization. WMA, wall motion abnormality; ED, Emergency Department.
patients being evaluated for OOMI. Our results support that PoCUS detection of WMA early in a patient’s ED visit may have the poten- tial to expedite the diagnosis of OOMI among patients whose tropo- nins fall into a nondiagnostic category.
We acknowledge the difference in time from ED arrival to revascu- larization between patients with and without WMA may not solely be explained by PoCUS findings accelerating catheterization. It may be that patients with WMA presented more typically of ACS, had sustained active chest pain, or appeared sicker. However, we found that HEART scores and first elevated troponin were not significantly different be- tween patients with and without WMA. The presence of a WMA should be interpreted in the context of the patient presentation, including their clinical presentation, ECG abnormalities that may not meet STEMI criteria, and general gestalt.
Emergency physicians in this study were able to identify WMA on PoCUS in 61% of patients who ultimately required revascularization for OOMI. While identifying a WMA may require more advanced PoCUS skills [12], the advent of artificial intelligence and speckle tracing may facilitate the accurate detection of WMA. These advancements may allow emergency physicians without advanced training in PoCUS to de- tect even subtle WMA.
Future directions include robust measurement of test characteristics of WMA on PoCUS for OOMI when performed by an emergency physi- cian and prospective assessment of how protocolized early PoCUS can salvage myocardium in the management of patients with OOMI.
-
- Limitations
We recognize several limitations to our study. The retrospective de- sign is prone to selection bias and confounding. It was conducted at a single center with limited demographic variability which may limit gen- eralizability. Although our findings show a decrease in arrival to cathe- terization time in those with WMA when compared to those without WMA, we are unable to establish causation. However, the two groups had similar clinical and demographic characteristics. The decision to catheterize a patient for potential percutaneous coronary intervention may have some level of subjectivity. Given our definition of OOMI for this study relied on catheterization, the results are subject to incorpora- tion bias.
We do not have a unified protocol to determine which patients re- ceive PoCUS; it is dependent on the physician caring for the patient and their Comfort level with PoCUS. Moreover, the timing of when a PoCUS examination is performed may depend on other factors outside of the patient’s clinical picture, including the ED census and how early the emergency physician is able to assess the patient. This may partially account for why certain patients received a cardiac PoCUS before an el- evated troponin result while others did not. Alternatively, more ill- appearing patients or patients presenting at low censUS times may have received an earlier or more extensive workup including PoCUS. Some physicians consistently incorporate early PoCUS into their clinical care, while others do not. It is likely that all these factors contribute to the timing of PoCUS performance, or even if a PoCUS is performed at all. Protocolizing PoCUS performance may minimize this variability and reveal an even clearer picture of the time advantage that PoCUS has over troponin results.
Although strongly discouraged, there may have been cardiac PoCUS exams performed without patient identifiers which would have other- wise met inclusion criteria. Patients scanned by operators noncompliant with the PoCUS workflow could not be included in our analysis due to the inability to perform a chart review. Ultimately, a multicenter, pro- spective study would be needed to address these limitations.
In our study PoCUS was performed significantly earlier than the time of troponin elevation among ED patients being evaluated for OOMI.
Patients with WMA were more expeditiously revascularized. Cardiac PoCUS may have a valuable role in the early diagnosis and treatment of OOMI. A larger prospective study is needed to validate our study findings.
Funding
None.
Author contributions
CX, AM, TN, MKH: Data curation. CX, JD, MKH: formal analysis. CX, AM, TN, JE, AA, JD, MKH: writing-original draft . CX, AM, TN, JE, AA, JD, MKH: writing-review & editing. CX, JD, MKH: Methodology. MKH: Conceptualization.
Credit authorship contribution statement
Curtis Xu: Writing – review & editing, Writing – original draft, Meth- odology, Formal analysis, Data curation. Andrew Melendez: Writing – review & editing, Writing – original draft, Data curation. Thuy Nguyen: Writing – review & editing, Writing – original draft, Data curation. Justin Ellenberg: Writing – review & editing, Writing – original draft, Data curation. Ambika Anand: Writing – review & editing, Writing – original draft. Joao Delgado: Writing – review & editing, Methodology, Formal analysis. Meghan Kelly Herbst: Writing – review & editing, Writing – original draft, Methodology, Formal analysis, Data curation, Conceptualization.
Declaration of Competing Interest
None.
Acknowledgements
The authors would like to thank Timothy Herbst MD, Geneva Hargis PhD, and Christopher “Kit” Bonin PhD for their assistance in reviewing and editing this manuscript.
This research did not receive any specific grant from funding agen- cies in the public, commercial, or not-for-profit sectors.
References
- Meyers HP, Bracey A, Lee D, Lichtenheld A, Li WJ, Singer DD, et al. Comparison of the ST-elevation myocardial infarction vs. NSTEMI and occlusion MI (OMI) vs. NOMI paradigms of acute MI. J Emerg Med. 2021 Mar;60(3):273-84.
- Scott IA. “time is muscle” in reperfusing occluded coronary arteries in acute myocar- dial infarction. Med J Aust. 2010 Nov 1;193(9):493-5. https://doi.org/10.5694/j. 1326-5377.2010.tb04030.x. [PMID: 21034380].
- Hauser AM, Gangadharan V, Ramos RG, Gordon S, Timmis GC, Dudlets P. Sequence of mechanical, electrocardiographic and clinical effects of repeated coronary artery oc- clusion in human beings: echocardiographic observations during coronary angio- plasty. J Am Coll Cardiol. 1985;5(2):193-7.
- Saglam C, Unluer EE, Yamanoglu NGC, et al. Accuracy of emergency physicians for detection of regional wall motion abnormalities in patients with chest pain without ST-elevation myocardial infarction. J Ultrasound Med. 2021 Jul;40(7):1335-42.
- Frenkel O, Riguzzi C, Nagdev A. Identification of high-risk patients with acute coro- nary syndrome using point-of-care echocardiography in the ED. Am J Emerg Med. 2014 Jun;32(6):670-2.
- Rong K, Chimileski B, Kaloudis P, Herbst MK. Impact of an epic-integrated point-of- care ultrasound workflow on ultrasound performance, compliance, and potential revenue. Am J Emerg Med. 2021 Jun 7;49:233-9. https://doi.org/10.1016/j.ajem. 2021.06.009. Epub ahead of print. 34146922.
- Croft PE, Strout TD, Kring RM, Director L, Vasaiwala SC, Mackenzie DC. WAMAMI: emergency physicians can accurately identify wall motion abnormalities in acute myocardial infarction. Am J Emerg Med. 2019 Dec;37(12):2224-8. https://doi.org/ 10.1016/j.ajem.2019.03.037. Epub 2019 Apr 3. PMID: 30987914.
- Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Executive group on behalf of the joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/world heart federation (WHF) task force for the Universal Definition of Myocardial Infarction. Fourth uni- versal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018 Oct 30;
72(18):2231-64. https://doi.org/10.1016/j.jacc.2018.08.1038. Epub 2018 Aug 25.
30153967.
- Daubert MA, Jeremias A. The utility of troponin measurement to detect myocardial infarction: review of the current findings. Vasc Health Risk Manag. 2010;6:691-9. Published 2010 Sep 7. https://doi.org/10.2147/vhrm.s5306.
- Giannitsis E, Katus HA. Cardiac troponin level elevations not related to acute coro- nary syndromes. Nat Rev Cardiol. 2013;10:623-34.
- Aslanger EK, Yildirimturk O, Simsek B, Bozbeyoglu E, Simsek MA, Yucel Karabay C, et al. DIagnostic accuracy oF electrocardiogram for Acute coronary occlusion
resuLTing in myocardial infarction (DIFOCCULT study). Int J Cardiol Heart Vasc. 2020 Jul 30;30:100603. https://doi.org/10.1016/j.ijcha.2020.100603. PMID:
32775606; PMCID: PMC7399112.
- Adhikari S, Fiorello A, Stolz L, Jones T, Amini R, Gross A, et al. Ability of emergency physicians with advanced echocardiographic experience at a single center to iden- tify complex echocardiographic abnormalities. Am J Emerg Med. 2014 Apr;32(4): 363-6. https://doi.org/10.1016/j.ajem.2013.12.010. Epub 2013 Dec 12. PMID:
24428984.
