Improper bystander-performed basic life support in cardiac arrests managed with public automated external defibrillators
a b s t r a c t
Aim: The aim of the study was to determine the quality of basic life support (BLS) in out-of-hospital cardiac arrests (OHCAs) receiving bystander cardiopulmonary resuscitation (CPR) and public Automated external defibrillator application.
Methods: From January 2006 to December 2012, data were prospectively collected from OHCA) and impending cardiac arrests treated with and without public AED before emergency medical technician (EMT) arrival. Basic Life support actions and outcomes were compared between cases with and without public AED application. Interruptions of CPR were compared between 2 groups of AED users: health care provider (HCP) and non-HCP. Results: Public AEDs were applied in 10 and 273 cases of impending cardiac arrest and non-EMT-witnessed OHCAs, respectively (4.3% of 6407 non-EMT-witnessed OHCAs). Defibrillation was delivered to 33 (13.3%) cases. Public AED application significantly improved the rate of 1-year Neurologically favorable survival in bystander CPR-performed cases with shockable initial rhythm but not in those with nonshockable rhythm. emergency calls were significantly delayed compared with other OHCAs without public AED application (median: 3 and 2 minutes, respectively; P b .0001). Analysis of AED records obtained from 136 (54.6%) of the 249 cases with AED application revealed significantly lower rate of compressions delivered per minute and significantly greater proportion of CPR pause in the non-HCP group. Time interval between power on and the first electrocardiographic analysis widely varied in both groups and was significantly prolonged in the non-HCP group (P = .0137).
Conclusions: Improper BLS responses were common in OHCAs treated with public AEDs. Periodic training for proper
BLS is necessary for both HCPs and non-HCPs.
(C) 2014
automated external defibrillators (AEDs) are designed for use by laypersons that have ideally been trained in basic life support (BLS). In Japan, both health care providers and citizens have been trained in the use of AEDs in BLS courses since the introduction of AEDs in 2004 [1]. Every year, more than 2% of the population is estimated to participate in the BLS training courses conducted by fire departments [2], authorized driving schools [3], Japanese Red Cross, and other associations.
Basic life support performers using AEDs should take care to minimize interruptions in chest compressions [4-6], particularly in cardiac arrests with nonshockable electrocardiographic rhythms, because good
? Conflicts of interest: We have no conflicts of interest to disclose.
* Corresponding author. Departments of Emergency Medical Science and emergency medical center, Kanazawa University Graduate School of Medicine, 13-1 Takaramachi, Kanazawa, 920-8641, Japan. Tel.: +81 76 265 2825; fax: +81 76 234 4243.
E-mail addresses: [email protected] (T. Nishi), [email protected] (Y. Takei), [email protected] (T. Kamikura), [email protected] (K. Ohta),
[email protected] (M. Hashimoto), [email protected] (H. Inaba).
quality chest compressions without delay or interruption are of primary importance in these patients [7-12]. Previous studies have suggested that interruptions of chest compressions because of AED voice prompts and rhythm analyses may be detrimental, particularly for patients with standard emergency medical service Response times of greater than 5 minutes [9-15]. Furthermore, application of an AED may cause the delay in placing emergency call and initiating cardiopulmonary resuscitation (CPR) when bystanders give preference to application of an AED over CPR [16]. Therefore, application of AEDs may cause poor BLS responses to OHCAs, particularly those related to the first 2 links in the chain of survival [4,5].
The number of public AEDs has increased in Japan [17], presumably because of the increased mass media reports of successful cases, increased layperson’s willingness to use a public AED [18], and conse- quent perceptions that AED installations are essential for public safety. Nevertheless, the quality of bystander-performed BLS with public AEDs has not been investigated in population-based study in Japan. Furthermore, the entire qualities of bystander-provided BLS including early emergency call and cardiopulmonary resuscitation have never
http://dx.doi.org/10.1016/j.ajem.2014.10.018
0735-6757/(C) 2014
been compared between cases with and without AED application in population-based study.
In this 7-year survey, we compared BLS responses between out-of- hospital cardiac arrests (OHCAs) treated with and without public AEDs. Also, we compared the interruptions of chest compressions between OHCAs treated by health care providers (HCPs) and non-HCP.
- Materials and methods
Data were collected in accordance with the national ethics guidelines for epidemiological surveys (The Ministry of Health, Labor and Welfare in Japan: http://www.mhlw.go.jp/general/seido/kousei/i-kenkyu/index. html). This study was approved by the review board of the Ishikawa Medical Control Council.
Populations and setting
The Ishikawa prefecture encompasses a snowfall area of 4186 km2 on the coast of the Sea of Japan and has a resident population of 1162953. The prefecture is divided into 4 administrative regions, including a central/urban region and 3 semirural/rural regions. In addition, 62% residents are located in the central urban region, which has an area of 1432 km2; and the rural population comprises older individuals compared with those in urban regions (30.1% vs 21.7% aged N 65 years, respectively).
Since the beginning of 2004, telephone-assisted CPR (telephone-CPR) has been conducted by all fire departments. Dispatchers instruct the method of performing compression-only CPR to callers unless bystanders are HCPs or well trained for providing BLS. Emergency medical techni- cians (EMTs) resuscitate patients experiencing OHCAs according to the protocol developed by the Ishikawa Medical Control Council, unless the patients exhibit postmortem changes. The EMT protocol is based on the guidelines of the American Heart Association and the Japan Resuscitation Council. Paramedics are authorized to perform the following procedures during resuscitation: (1) the use of suprapharyngeal airways, (2) infusion of Ringer’s lactate via a peripheral vein, and (3) the use of semiautomated external defibrillators. Since July 2004, specially trained paramedics have been permitted to insert tracheal tubes under limited indication criteria; and since April 2006, they have been permitted to administer intrave- nous adrenaline. However, EMTs are not permitted to terminate resusci- tation in the field.
The total number of participants in BLS training courses conducted by fire departments and authorized driving schools were 38 315 in 2006, 35668 in 2007, 33346 in 2008, 34587 in 2009, 32875 in 2010,
and 33727 in 2011. These annual numbers correspond to approximately 3% of the population in the Ishikawa prefecture. All BLS courses were conducted according to Japan Resuscitation Council BLS Guidelines (http://jrc.umin.ac.jp/pdf/20121005_BLS.pdf), which emphasize the importance of chest compressions.
The total number of public AEDs in Ishikawa prefecture was 555, 1786, and 2534 at the end of 2007, 2009, and 2011, respectively. Approximately 220 public AEDs per 100000 people were installed at the end of 2011. Each fire department in Ishikawa prefecture organized a public campaign event for use of AED at least once a year.
Patient data and analysis of BLS responses and interruptions of chest compressions
During the study period of January 2006 to March 2012, data were prospectively collected from OHCAs that were not witnessed by EMTs (non-EMT-witnessed OHCAs). After application of public AEDs, staff or EMTs in each fire department collected ECG and AED application records, whenever possible.
The collected patient data were based on the Utstein template and included backgrounds of OHCAs (location, region, patient’s age, patient’s sex, arrest witness, possible causes of arrest, bystander CPR,
initial cardiac rhythm, defibrillation delivered, and public AED user), time factors [estimated time interval between collapse and CPR initia- tion by bystanders and time interval between the emergency call and EMT arrival at the scene (recorded in seconds)]. The outcomes measured were sustained return of spontaneous circulation (SROSC), one-year (1-Y) survival, and 1-Y neurologically favorable survival. Sustained return of spontaneous circulation was defined as the continuous presence of pal- pable pulses for more than 20 minutes. The 1-Y survival rate was defined as the patient being alive in a hospital, at home, or in a care or rehabilita- tion facility at 1 year. Cerebral Performance Categories (CPCs) were eval- uated after resuscitation. The 1-Y neurologically favorable survival was defined as CPC of 1 (good recovery) or 2 (moderate disability) in patients without neurological disturbances before the arrest event and when the best CPC was equal to the prearrest category in patients with neurological disturbances. The primary end point was 1-Y neurologically favorable sur- vival. The secondary end points were SROSC and 1-Y survival.
Analysis of interruptions of chest compressions in cases with
ECG records was manually determined with reference to the episode duration [19,20]. Time intervals were recorded from public AED power on to initial analysis, emergency call to public AED power on, arrest witness/recognition to first AED analysis, public AED power on to the end of bystander CPR, rates of chest compressions, fraction of time intervals with compression rate less than 90 or greater than 120 min, compressions delivered per minute, No-flow times (pauses), proportion of BLS pause (excluding the time for analysis), and number of pauses of more than 10 seconds within 1-minute segments.
Statistical analysis
Data were analyzed using JMP ver.10 for Windows (SAS institute, Cary, NC). The ?2 test with or without Pearson correction was applied for univariable analyses. The Kruskal-Wallis test was used for nonpara- metric comparisons. Multivariable logistic regressions were performed to identify factors associated with outcomes. Differences and correlations were considered significant when P b .05. Adjusted odds ratio (OR) and 95% confidence interval (CI) were calculated using profile likelihood.
- Results
- Overview of public AED applications in non-EMT-witnessed OHCAs and consequent outcomes
During the study period, 6407 OHCA cases were witnessed by citizens in the absence of EMTs. Of these, public AED were applied in 273 (4.3%) cases and were attached to 10 non-OHCA cases wherein arrest was not confirmed by citizens or EMTs (Fig. 1). Number of public AED applications increased with the increased number of public AEDs: 17, 58, and 104 cases during 2006-2007, 2008-2009, and 2010-2011, respectively. When maximally estimated, the utilization ratio of public AEDs did not largely change during the study period: 3.1% (17/555), 3.2% (58/1786), and 4.1% (104/2534) during 2006-2007, 2008-2009,
and 2010-2011, respectively.
In 24 of 273 cases of non-EMT-witnessed OHCA with public AED application, AEDs were applied; but bystanders did not initiate CPR. However, bystander CPR was performed in 249 (91.2%) of these cases and was performed in 3491 (56.9%) of 6134 cases of non-EMT- witnessed OHCA without public AEDs (P b .0001); of these 249 cases, 216 had no defibrillation with public AED before EMT arrival at patients. Furthermore, AED application and ECG records were collected in 136 (55%) of these 249 cases. In the remaining cases, AED application records had been deleted before the EMTs requested for them. The AEDs applied to OHCA cases did not have a CPR-feedback function.
The proportion of any ROSC before EMT arrival at patients was 2.8% and 0.4% in cases with application of public AED and those without the application, respectively (P b .0001). Public AED application significantly improved overall outcomes of non-EMT-witnessed, bystander CPR-
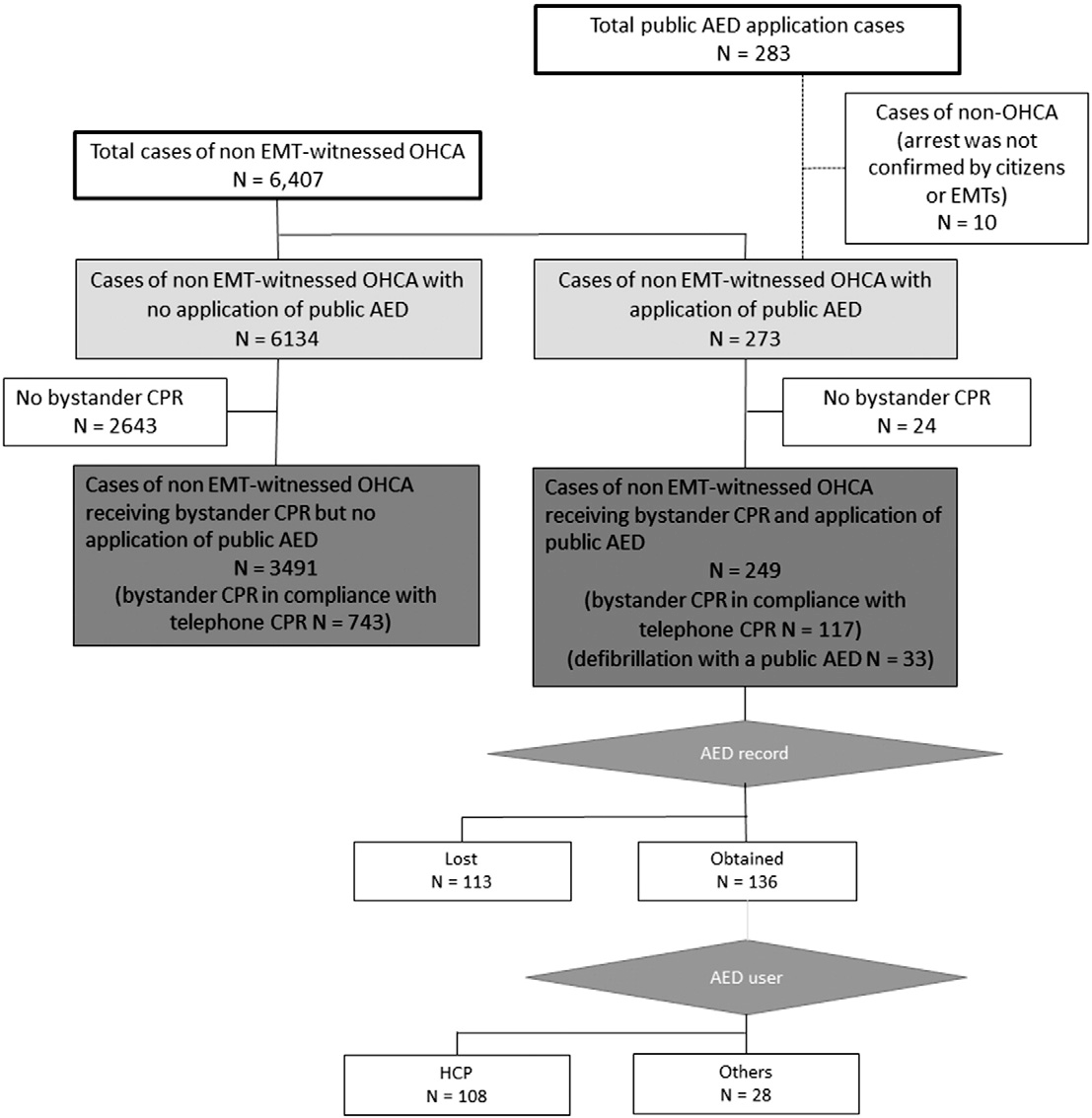
Fig. 1. Overview of data collection and analysis.
performed OHCAs (Table 1). However, when subgroup analysis for initial rhythm was performed (Fig. 2), application of public AED augmented the rate of 1-Y neurologically favorable survival only in the subgroup with shockable initial rhythm.
Differences in characteristics and backgrounds between the 2 groups of non-EMT-witnessed, bystander CPR-performed OHCAs with and without public AED
Public AEDs were applied in 249 (6.7%) of 3740 cases of non-EMT- witnessed bystander-performed CPR OHCA (Table 1). Public AEDs were more frequently used at care facilities (unadjusted OR; 95% CI: 16.256; 11.868-22.268) and in OHCAs of presumed cardiac etiology (1.390; 1.075-1.797). Patients were older (P b .0001) and were predominantly female (0.750; 0.580-0.969) in the group receiving public AEDs. Public AEDs were used by HCPs in 206 (82.7%) of 249 cases. Emergency medical technicians performed the first defibrillation with their own AED in 481 (13.8%) of 3491 cases without public AEDs and the first or additional defibrillation in 30 (11.9%) of 249 cases with public AEDs. Furthermore, bystander CPR was less frequently initiated in compliance with telephone-CPR in cases with public AEDs (0.306; 0.236-0.398). Bystander CPR was more frequently conventional (chest compressions and ventilations) in public AED-treated cases (2.600; 1.958-3.452).
Time intervals between witness of arrest and emergency call (P b .0001) and between emergency call and EMT arrival (P b .0001) were significantly longer, whereas the time interval between witness of arrest and bystander CPR (P b .0001) was significantly shorter, in the public AED-treated group.
Differences in backgrounds of OHCA, BLS time factors, and OHCA outcomes between HCP- and non-HCP-witnessed OHCA cases with ECG records (Table 2)
Health care providers predominantly used AEDs in care facilities (102/108), whereas non-HCPs used them only in public locations (28/28). Patient age was significantly higher in the HCP group than in the non-HCP group (P b .0001). Moreover, shockable initial rhythms were more frequently recorded (unadjusted OR; 95% CI: 2.923; 1.070- 7.978) and defibrillation with public AEDs was less frequently performed (2.973; 1.172-7.540) in the non-HCP group than in the HCP group.
No significant differences were observed in BLS time factors, witness and recognition to call (P = .0594), emergency call to arrival at the scene (P = .7044), witness/recognition to bystander CPR (P = .4249), or witness/recognition to AED power on (P = .3673). Notably, lower interquartile values of call to AED power on times were negative; that is, in 43 of 108 cases in the HCP group and in 5 of 28 cases in the non-
Differences in characteristics and backgrounds between the 2 groups of non-EMT-witnessed OHCAs receiving bystander CPR with and without public AED application Characteristics, backgrounds, and outcomes Public AED application P value (univariate analysisa) OR (95% CI) for public AED application
|
No (n = 3491) |
Yes (n = 249) |
(univariate analysis) |
||
|
Location, % (n) |
||||
|
Care facilities |
18.8% (655) |
79.0% (199) |
b.0001 |
16.256 (11.868-22.268) |
|
Region, % (n) |
||||
|
Central |
47.1% (1643) |
48.8% (123) |
.5921 |
1.072 (0.830-1.386) |
|
Patient’s age, median (25%-75%) |
79 (68-86) |
84 (72-90) |
b.0001 |
Undefined |
|
Patient’s sex, % (n) |
||||
|
Male |
55.6% (1940) |
48.4% (122) |
.0278 |
0.750 (0.580-0.969) |
|
Etiology, % (n) Presumed cardiac |
45.8% (1597) |
54.0% (136) |
.0116 |
1.390 (1.075-1.797) |
|
Arrest, % (n) |
||||
|
Witnessed |
37.0% (1292) |
38.1% (96) |
.7308 |
1.047 (0.804-1.362) |
|
Initial rhythm, % (n) Shockable |
8.3% (289) |
10.7% (27) |
.1944 |
1.329 (0.876-.017) |
|
Defibrillation with public AED, % (n) Performed |
None |
13.1% (33) |
Undefined |
Undefined |
|
Any ROSC before EMT arrival at patients |
0.4% (14) |
2.8% (7) |
b.0001 |
7.184 (2.873-17.965) |
|
Public AED user, % (n) HCP |
None |
82.7% (206) |
Undefined |
Undefined |
|
Type of CPR before EMT arrival, % (n) |
||||
|
Chest compression and ventilation 14.9% (521) |
31.3% (78) |
b.0001 |
2.600 (1.958-3.452) |
|
|
Origin of CPR before EMT arrival, % (n) |
||||
|
In compliance with telephone-CPR |
78.6% (2745) |
53.0% (132) |
b.0001 |
0.306 (0.236-0.398) |
|
EMT-performed defibrillation after their arrival at patients |
13.8% (481) |
11.9% (30) |
.3946 |
0.845 (0.570-1.253) |
|
Time interval, median (25%-75%) Witness/recognition to call (min) |
2 (1-5) |
3 (1-7) |
b.0001 |
Undefined |
|
Emergency call to EMT arrival at patient (s) |
453 (355-590) |
523 (419-632) |
b.0001 |
Undefined |
|
Witness/recognition to bystander CPR (min) |
2 (1-5) |
1 (1-4) |
b.0001 |
Undefined |
|
Outcomes, % (n) SROSC |
27.7% (968) |
38.6% (96) |
.0004 |
1.635 (1.253-2.133)b |
|
1-Y survival |
6.5% (226) |
9.2% (23) |
.1077 |
1.470 (0.937-2.305)b |
|
1-Y neurologically favorable survival |
3.4% (118) |
7.6% (19) |
.0022 |
2.361 (1.428-3.903)b |
|
a ?2 test with or without Pearson correction. |
||||
b Adjusted OR (95% CI) with no public AED application as reference, obtained by multivariable logistic regression including etiology of arrest (presumed cardiac or noncardiac), initial rhythm (shockable or not), witnessing of arrest (witnessed or not), and response time (emergency call to EMT arrival at patients), was 1.687 (1.264-2.242), 1.467 (0.862-2.392), and 2.492 (1.350-4.400) for ROSC, 1-Y survival, and neurologically favorable 1-Y survival, respectively.
HCP group, public AEDs were powered on before the emergency call was made.
Return of spontaneous circulation was obtained before EMT arrival in 3 cases in the HCP group and in 1 case in the non-HCP group (P = .8287). No significant differences in overall outcomes of OHCA (sustained ROSC, P = .6374; 1-Y survival, P = .5164; or 1-Y neurologically favorable survival, P = .2831) were observed between the 2 groups.
Comparisons of AED-related critical time factors (Table 3 & Fig. 3)
Analyses of CPR quality in 136 cases with ECG records revealed that compression rates (P = .0187), the duration of compression rates (P = .0124), and the number of compressions delivered per minute (P = .0008) were significantly lower in the non-HCP group than the HCP group. Furthermore, no-flow times per 1-minute segment (P = .0067), the proportion of chest compression pause (P = .0474), and CPR pauses (P = .0116) significantly differed between both groups. As presented in Fig. 3, the time interval from power on to the first ECG analysis varied widely in both groups. However, this time interval was significantly prolonged in the non-HCP group (P = .0212), with median values (10%-90%) of 39.5 (4-69) and 49 (10-124) seconds in the HCP and non-HCP groups, respectively. This interval exceeded 60 seconds in 20 of 108 cases in the HCP group and in 10 of 28 cases in the non-HCP group. The AED pad was changed in at least 2 cases
because of improper attachment.
Automated external defibrillators are designed for use by laypersons who have ideally been trained in BLS. Basic life support providers using
AEDs should take care to minimize interruptions in chest compressions [4-6], particularly during cardiac arrests with nonshockable ECG rhythms. In this study, AED application significantly improves overall outcomes of non-EMT-witnessed, bystander CPR-performed OHCAs with shockable initial rhythm but not those with nonshockable initial rhythm. Also, we showed that HCPs provide a higher Quality of CPR in public AED-treated cases.
Public AEDs were most frequently applied (77.4%) in care facilities, where OHCA patients were reported to be mostly elderly women with disabilities or illnesses and less shockable initial rhythms [16,21-24]. Survival rates after OHCAs in care facilities are reportedly low [25,23]. In addition, among out-of-home OHCAs, 48% and 34% to 39% occur in health care-related locations and extended-care facilities, respectively [23,26]. We have reported that layperson’s knowledge on how to use an AED and their willingness to use an AED increased during the study period, presumably because of the increased number of reports on successful resuscitation by citizens using the AED [18]. To enhance the beneficial effects of public AEDs, public AEDs should be increased in public locations other than care facilities [17].
Increased time interval from emergency call to EMT arrival reportedly led to poorer OHCA outcomes [27,28]. As presented in Table 1, this time factor interval in the public AED-treated group was significantly longer than that in AED-untreated group. However, the time intervals from arrest witness/recognition to bystander CPR were shorter in the public AED-treated group, indicating that early CPR was more frequently performed by trained bystanders in these cases. Furthermore, HCPs more frequently performed bystander CPR on their own initiative (independent of telephone-CPR) in the public AED-treated group. In addition, SROSC due to defibrillation with public AEDs before EMT arrival might contribute towards better OHCA outcomes. In fact, public
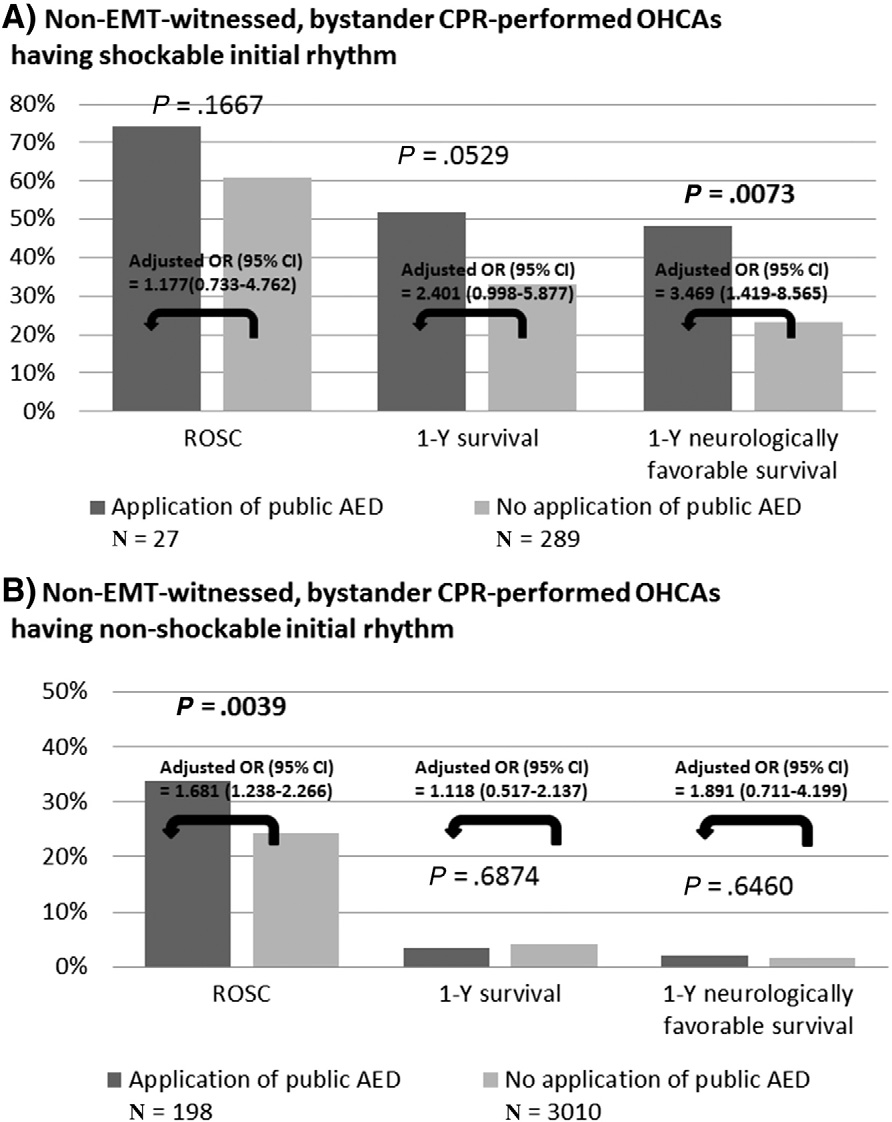
Fig. 2. Comparisons of outcomes between the public AED application group and the nonapplication group. Adjusted ORs for outcomes with no public AED application as reference, obtained by multivariable logistic regression including etiology of arrest (presumed cardiac or noncardiac), arrest witness (witnessed or not), and response time (emergency call to EMT arrival at patients) were shown.
application of AEDs significantly augmented 1-Y survival from non-EMT- witnessed, bystander CPR-performed OHCAs.
Although it is legal for non-HCP bystanders to apply AEDs in Japan and the number of AEDs has increased [17,18], only 33 (14.5%) of 249 cases involved a non-HCP AED user. When non-HCP bystanders used AEDs, the incidence of shockable initial rhythms was significantly higher (28.6% vs 12.0%, .0424); but the Quality of chest compressions was lower. The large proportion of interruption of chest compressions may have prevented differences in OHCA outcomes between the HCP and non-HCP group.
This study discloses the unfavorable issues related to BLS responses to OHCA cases treated with public AEDs. First, disordered sequences of survival actions such as AED use prior to emergency calls and delays in placing emergency call [16,26,29,30] are common when public AEDs are used. Time intervals from witness/recognition of arrest to emergency calls were significantly prolonged (Table 1). The lower interquartile value of emergency call to AED power on time intervals was negative (Table 3), and emergency calls were made after powering on public AEDs in 35.3% [(43 + 5)/(18 + 28)] of AED-treated cases.
Second, the time interval between AED power on and initial analysis was occasionally prolonged. First use of unfamiliar public AEDs, improper placement of AED pads because of age, and the hesitation to expose chests and washboard-like chest walls of patients with cachexia are
proposed as the reasons for considerable delays in initial analyses. It is assumed that chest compressions may be interrupted or ceased during this time period. In most BLS training courses, students are trained in the placement of AED pads on manikins, which have easily exposed chests; and little attention is paid to the importance of tight placement. These issues in BLS training may also cause delays.
There are several limitations in this study. Although staff and EMT in all fire departments made every effort to collect ECG and AED applica- tion records, they failed to collect these records in 113 out of 249 public AED-treated cases. Furthermore, the depth of chest compressions or other CPR components, including airway management [31], was not evaluated in this study. Therefore, quantitative analyses of the quality of chest compressions or CPR are incomplete and may not be represen- tative of all cases of treatment with public AEDs. Health care providers primarily used AEDs in care facilities, whereas non-HCPs used it only in other public facilities. Therefore, our observations depended on OHCA locations as well. Automated external defibrillators with CPR- feedback functions were introduced in our region in 2012. No AED applied in OHCA cases had the CPR-feedback function. Therefore, effects of this feedback system on the interruption of chest compressions or other BLS actions were not evaluated in this study.
Improper BLS responses were common in OHCAs treated with public AEDs. Some citizens may give higher priority to AEDs over other BLS
Differences in backgrounds, characteristics, and outcomes between HCP and non-HCP in cases with AED record
Characteristics and backgrounds AED record obtained (n = 136)
Public AED user
HCP
(n = 108)
Non-HCP (n = 28)
P value (univariate analysisa) OR (95% CI) for obtained AED record
(univariate analysis)
Region, % (n)
|
Location, % (n) |
||||
|
Care facilities 94.4% (102) |
0% (0) |
b.0001 |
Undefined |
|
|
Central 63.9% (69) |
60.7% (17) |
.7570 |
0.874 (0.371-2.053) |
|
|
Patient’s age, median (25%-75%) |
84 (77-89) |
59 (47-74) |
b.0001 |
Undefined |
|
Patient’s sex, % (n) |
||||
|
Male |
50.0% (54) |
57.1% (16) |
.4996 |
1.333 (0.576-3.082) |
|
Etiology of arrest, % (n) |
||||
|
Presumed cardiac |
61.1% (66) |
57.1% (16) |
.7030 |
0.848 (0.365-1.970) |
|
Arrest witness, % (n) |
||||
|
Witnessed |
32.4% (35) |
53.6% (15) |
.0414 |
2.406 (1.033-5.602) |
|
Initial rhythm, % (n) |
||||
|
Shockable rhythm |
12.0% (13) |
28.6% (8) |
.0424 |
2.923 (1.070-7.978) |
|
Defibrillation with an public AED, % (n) |
15.7% (17) |
35.7% (10) |
.0251 |
2.973 (1.172-7.540) |
|
Type of CPR before EMT arrival, % (n) |
||||
|
Chest compression and ventilation |
32.4% (35) |
10.7% (3) |
.0143 |
0.250 (0.070-0.885) |
|
Origin of CPR before EMT arrival, % (n) |
||||
|
In compliance with telephone-CPR |
46.3% (50) |
57.1% (16) |
.3058 |
1.547 (0.668-3.584) |
|
Time interval, median (25%-75%) witness/recognition to call (min) |
4 (1-7) |
3 (1-5) |
.0594 |
Undefined |
|
Call to EMT arrival at patient (s) |
526 (421-631) |
487 (401-647) |
.7044 |
Undefined |
|
Witness/recognition to bystander CPR (min) |
1 (1-3) |
1 (1-4) |
.4249 |
Undefined |
|
Witness/recognition to public AED power on |
5 (2-9) |
4 (2-7) |
.3673 |
Undefined |
|
Call to public AED power on |
1 (-1 to 3) |
2 (0-4) |
.2363 |
Undefined |
|
Outcomes, % (n) ROSC before EMT arrival |
2.8% (3) |
3.6% (1) |
.8287 |
0.771 (0.077-7.752) |
|
Sustained ROSC |
38.0% (41) |
42.9% (12) |
.6374 |
0.816 (0.351-1.898) |
|
1-Y survival |
13.0% (14) |
17.9% (5) |
.5164 |
0.685 (0.224-2.096) |
|
1-Y neurologically favorable survival |
10.2% (11) |
17.9% (5) |
.2831 |
0.522 (0.165-1.650) |
|
a ?2 test with or without Pearson correction. |
||||
Comparisons of AED-related time factors and CPR quality parameters between HCP and non-HCP in cases with AED record
|
Time factor |
ECG record collected (n = 136) |
P value by univariate analysis |
|
|
Public AED user |
|||
|
HCP |
Non-HCP |
||
|
(n = 108) |
(n = 28) |
||
|
Episode duration (power on to the end of bystander CPR) |
|||
|
Episode mean |
462 |
366 |
.0513 |
|
Episode median (25%-75%) |
433 (251-626) |
284 (190-546) |
|
|
Compression rate Episode median (25%-75%) |
109.5 (99-121) |
103 (86.5-113) |
.0187 |
|
Fraction of minutes with compression rate |
|||
|
b90/min |
9% (10) |
29% (8) |
.0124 |
|
90-120/min |
64% (69) |
61% (17) |
|
|
N 120/min |
27% (29) |
11% (3) |
|
|
Compression delivered per minute Episode mean |
72 |
55 |
.0008 |
|
Episode median (25%-75%) |
74 (61-86) |
63 (37-74) |
|
|
No-flow time (pauses), s |
|||
|
Mean no-flow time |
137 |
128 |
.6651 |
|
Median no-flow time (25%-75%) |
116 (57-192) |
110 (48-205) |
|
|
Median analyze pause (25%-75%) |
35 (24-58) |
25 (16-53) |
.2547 |
|
Median postanalyze pause (25%-75%) |
68 (33-147) |
54 (24-152) |
.6689 |
|
No-flow time per 1-min segment |
19 (14-27) |
25 (17-35) |
.0067 |
|
Proportion of CPR pause (except for analyze time), % Median compression pause (25%-75%) |
23 (14-37) |
33 (18-51) |
.0474 |
|
Median CPR pause (25%-75%) |
18 (10-32) |
31 (16-46) |
.0116 |
|
Number of N 10-s pause per 1 min segment Mean N 10-s pause |
0.71 |
0.81 |
.2847 |
|
Median N 10-s pause |
0.6 (0.5-0.8) |
0.7 (0.6-0.9) |
|
|
Median analyze pause (25%-75%) |
0.5 (0.4-0.6) |
0.5 (0.4-0.6) |
.3604 |
|
Median postanalyze pause (25%-75%) |
0.1 (0-0.3) |
0.2 (0-0.4) |
.7531 |
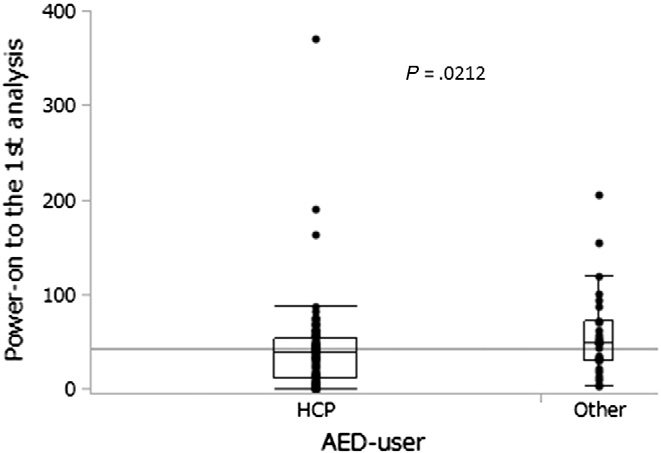
Fig. 3. Distribution of time intervals between AED power on and initial analysis. Boxes denote the interquartile range, and bars represent 95% CIs. The horizontal line represents the median value of all cases.
actions. High-quality CPR with minimal interruption of chest compres- sions was rarely performed in OHCAs managed by non-HCPs using public AEDs. To minimize the unfavorable effects of public-administered AEDs on OHCAs without shockable initial rhythms, periodic BLS training will be necessary for both HCPs and non-HCPs.
Acknowledgment
We thank all fire departments in the Ishikawa Prefecture for collection of data and AED records.
HI conceived and designed the study. TN, YT and TK collected, and analyzed the data. TN, KO, MH and HI interpreted the data. TN and HI drafted the manuscript, and all authors contributed substantially to its revision. HI provided administrative, technical and material support. TN takes responsibility for integrity of the data and accuracy of the data analysis.
- Ministry of Health, Labour and Welfare (Accessed 23 February, 2013, at http://www. mhlw.go.jp/english/ and http://www.mhlw.go.jp/shingi/2004/07/s0701-3.html).
- Fire and Disaster Management Agency. (Accessed on May 25, 2014, at http://www. fdma.go.jp/en/ and http://www.fdma.go.jp/neuter/topics/fieldList9_3_1.html).
- Driver’s license statistics. Accessed on May 25, 2014, at https://www.npa.go.jp/ toukei/menkyo/index.htm.
- Handley AJ, Koster R, Monsieurs K, Perkins GD, Davies S, Bossaert L. European Resus- citation Council guidelines for resuscitation 2005. Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation 2005;67:S7-S23.
- Berg RA, Hemphill R, Abella BS, Aufderheide TP, Cave DM, Hazinski MF. Part 5: adult basic life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2010;122:S685-705.
- JRC guidelines. Accessed 23 February, 2013, at http://www.qqzaidan.jp/pdf_5/ guideline1_BLS_kakutei.pdf.
- Barash DM, Raymond RP, Tan Q, Silver AE. A new defibrillator mode to reduce chest compression interruptions for health care professionals and lay rescuers: a pilot study in manikins. Prehosp Emerg Care 2011;15:88-97.
- Nolan JP, Soar J. Defibrillation in clinical practice. Curr Opin Crit Care 2009;15: 209-15.
- Sato Y, Weil MH, Sun S, Tang W, Xie J, Noc M, et al. Adverse effects of interrupting precordial compression during cardiopulmonary resuscitation. Crit Care Med 1997;25:733-6.
- Yu T, Weil MH, Tang W, Sun S, Klouche K, Povoas H, et al. Adverse outcome of interrupted precordial compression during automated defibrillation. Circulation 2002;106:368-72.
- Rea TD, Stickney RE, Doherty A, Lank P. Performance of chest compressions by lay- persons during the Public access defibrillation Trial. Resuscitation 2010;81:293-6.
- Babbs CF, Kemeny AE, Quan W, Freeman G. A new paradigm for human resuscitation research using intelligent devices. Resuscitation 2008;77:306-15.
- Eftestol T, Sunde K, Steen PA. Effects of interrupting precordial compressions on the calculated probability of defibrillation success during out-of-hospital cardiac arrest. Circulation 2002;105:2270-3.
- van Alem AP, Sanou BT, Koster RW. Interruption of cardiopulmonary resuscitation with the use of the automated external defibrillator in out-of-hospital cardiac arrest. Ann Emerg Med 2003;42:1-9.
- Steen S, Liao Q, Pierre L, Paskevicius A, Sjoberg T. The critical importance of minimal delay between chest compressions and subsequent defibrillation: a haemodynamic explanation. Resuscitation 2003;58:249-58.
- Takei Y, Nishi T, Takase K, Kamikura T, Inaba H. Misplaced links in the chain of survival due to an incorrect manual for the emergency call at public facilities. Int J Emerg Med 2013;6:33.
- National disaster medical center. Accessed 23 February, 2013, at http://aed-hyogo. sakura.ne.jp/wpm/archivepdf/23/2_11a.pdf.
- Enami M, Takei Y, Goto Y, Ohta K, Inaba H. The effects of the new CPR guideline on attitude toward basic life support in Japan. Resuscitation 2010;81:562-7.
- Kramer-Johansen J, Edelson DP, Losert H, Kohler K, Abella BS. Uniform reporting of measured Quality of cardiopulmonary resuscitation (CPR). Resuscitation 2007;74: 406-17.
- Ong ME, Annathurai A, Shahidah A, Leong BS, Ong VY, Tiah L, et al. Cardiopulmonary resuscitation interruptions with use of a load-distributing band device during emer- gency department cardiac arrest. Ann Emerg Med 2010;56:233-41.
- Tresch DD, Neahring JM, Duthie EH, Mark DH, Kartes SK, Aufderheide TP. Outcomes of cardiopulmonary resuscitation in nursing homes: can we predict who will benefit? Am J Med 1993;95:123-30.
- Shah MN, Fairbanks RJ, Lerner EB. Cardiac arrests in skilled nursing facilities: continuing room for improvement? J Am Med Dir Assoc 2006;7:350-4.
- Benkendorf R, Swor RA, Jackson R, Rivera-Rivera EJ, Demrick A. Outcomes of cardiac arrest in the nursing home: destiny or futility? Prehosp Emerg Care 1997;1:68-72.
- Ghusn HF, Teasdale TA, Pepe PE, Ginger VF. Older nursing home residents have a Cardiac arrest survival rate similar to that of older persons living in the community. J Am Geriatr Soc 1995;43:520-7.
- Portner ME, Pollack ML, Schirk SK, Schlenker MK. Out of hospital cardiac arrest loca- tions in a rural community where should we place AEDs? Prehosp Disaster Med 2004;19:352-5.
- Takei Y, Inaba H, Yachida T, Enami M, Goto Y, Ohta K. Analysis of reasons for emer- gency call delays in Japan in relation to location: high incidence of correctable causes and the impact of delays on patient outcomes. Resuscitation 2010;81:1492-8.
- Pell JP, Sirel JM, Marsden AK, Ford I, Cobbe SM. Effect of reducing ambulance response times on deaths from out of hospital cardiac arrest: cohort study. BMJ 2001;322:1385-8.
- O’Keeffe C, Nicholl J, Turner J, Goodacre S. Role of Ambulance response times in the survival of patients with out-of-hospital cardiac arrest. Emerg Med J 2011;28:703-6.
- Herlitz J, Engdahl J, Svensson L, Young M, Angquist KA, Holmberg S. A short delay from out of hospital cardiac arrest to call for ambulance increases survival. Eur Heart J 2003;24:1750-5.
- Swor RA, Compton S, Domeier R, Harmon N, Chu K. Delay prior to calling 9-1-1 is associated with increased mortality after out-of-hospital cardiac arrest. Prehosp Emerg Care 2008;12:333-8.
- Safar P, Bircher N, Prieto E, Berkebile P, Tisherman SA, Marion D, et al. Reappraisal of mouth-to-mouth ventilation. Ann Emerg Med 1998;31:653-4.
